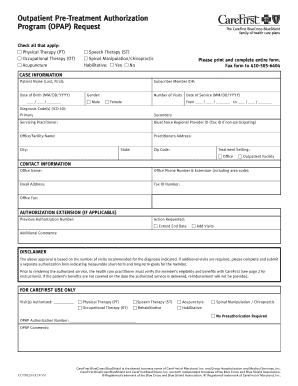
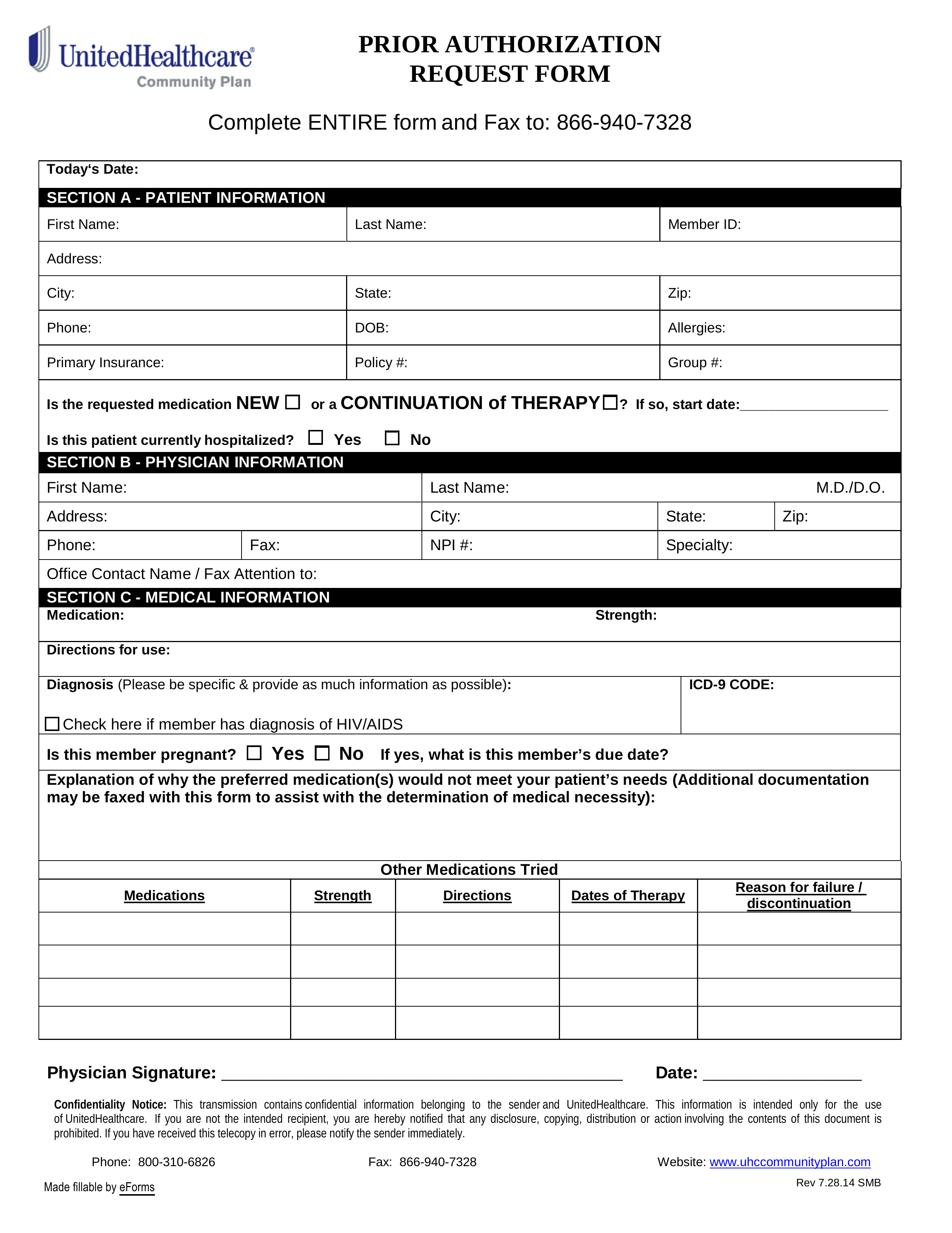
If your health plans formulary guide indicates that you need a Prior Authorization for a specific drug your physician must submit a prior authorization request form to the health plan for approval. 518 641-3784 Fax.
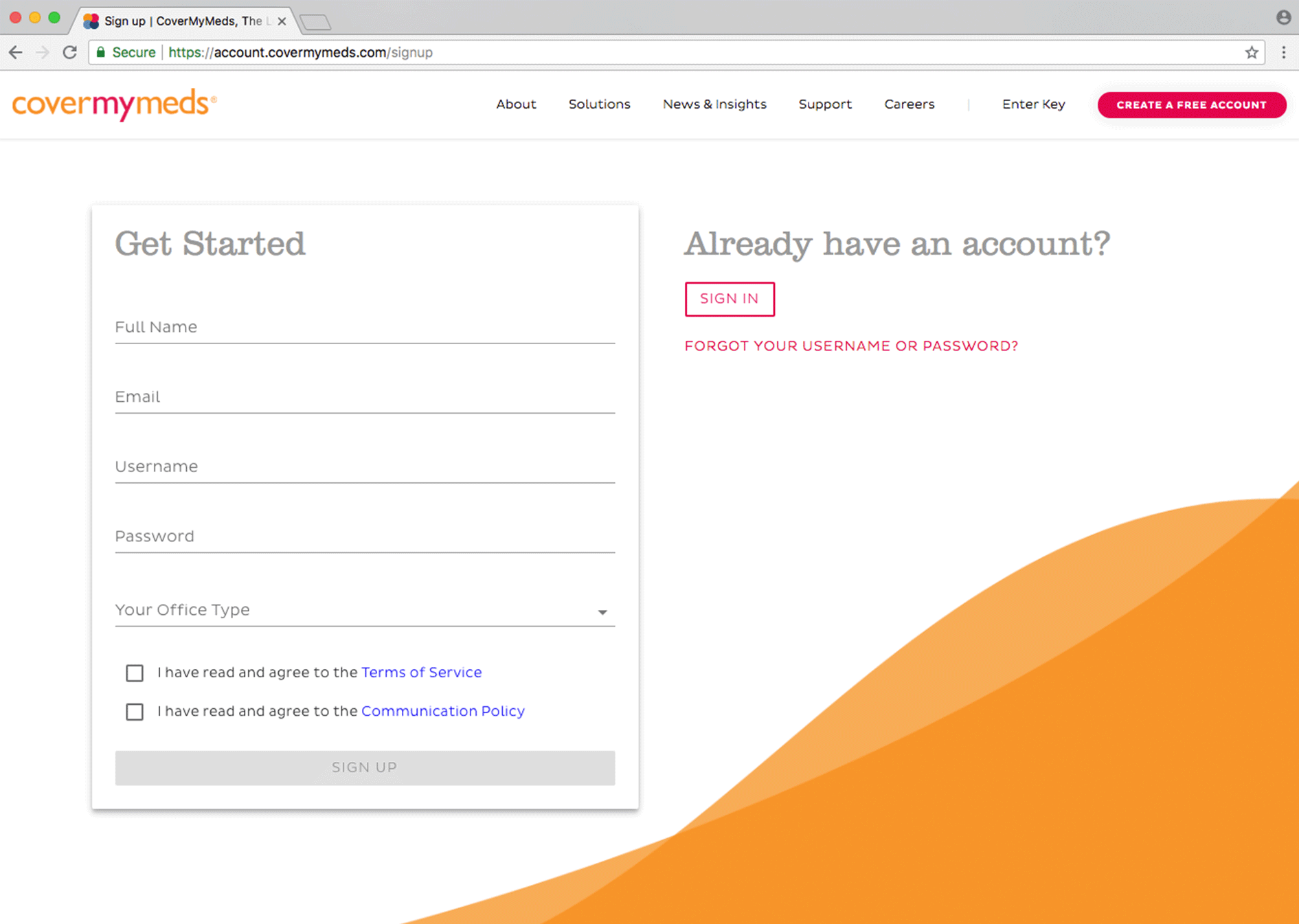 Prime Therapeutics Prior Authorization Forms Covermymeds
Prime Therapeutics Prior Authorization Forms Covermymeds
Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptionsA non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
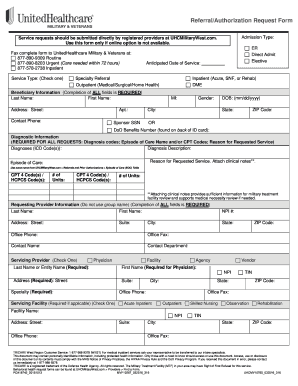
Php prime prior auth form. Getting prior authorization means youre getting the care approved by your regional contractor before you actually go to an appointment and get the care. This document will contain the diagnosis and an explanation for why the prescription is suggested above those which are potentially more commonly used. On the prior authorization form the person making the request must provide a medical rationale as to why the chosen medication is necessary.
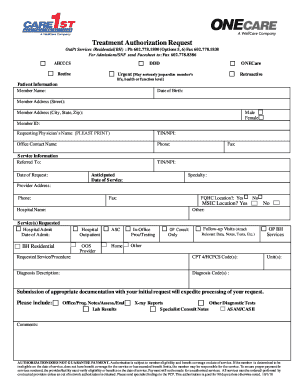
CDPHP Pharmacy Department 500 Patroon Creek Blvd Albany New York 12206-1057. PRIOR AUTHORIZATION REQUEST PRESCRIBER FAX FORM Only the prescriber may complete this form. PHYSICIANS HEALTH PLAN NOTIFICATIONPRIOR AUTHORIZATION TABLE-ALL PRODUCTS PHP NotificationPrior Approval Table-All Products Effective January 27 2021 Notification Requirement J1632 brexanolone 1 mg Zulresso J1640 panhematin Hemin J1675 histrelin acetate Vantas Supprelin LA J1738 meloxicam 1 mg Anjeso.
Incomplete forms will be returned for additional information. 2 is the only even prime number. Please note you do not need to sign a producer agreement in order to get a free quote.
Sleep Study Request Form. Below are documents that provide more information about PHPs authorization requirements and service listings. We want to provide the best service possible and need to know a little more about you so please complete the 1 Risk Summary and 2 Application.
Drugs Requiring Prior Authorization List. PHP NotificationPrior Approval Table. PHPprime is contracted with UnitedHealthcare to manage more than 25000 covered lives under their AARP Medicare Complete Medicare Advantage plan.
Home Health Care Request Form. You may also report directory errors by calling Provider Relations at 888 726-5411 between the hours of 800 am to 800 pm Monday through Friday. Numbers 2 3 5 7 11 13 17 etc.
If you wish to request coverage for a patients prescription which hasnt been listed on their health insurance providers formulary you will need to fill out a Prime Therapeutics Prior Authorization Form aka. Prior Authorization Request Form. Under this professional risk payment model PHPprime provides care coordination prior authorization quality improvement coaching network management risk adjustment coding.
Care to Care Fax Form. Request for Referral to Non-Participating Provider. Medication Prior Approval Form.
The Prior Authorization Department streamlines the process of referring your patients to specialists by. If you are unable to access the online forms Service Authorization requests and notification forms can be submitted using printable forms. CDPHP Prior Authorization Medical Exception Request Form Fax or mail this form back to.
PHPprime Care Home. DME Authorization Request Form. Prior Authorization Request Form.
It is a natural number greater than 1 and so 0 and 1 are not prime numbers. The following documentation is REQUIRED. Dental Service Authorization Requests Submit dental Service Authorization requests on American Dental Association ADA claim forms along with adequate and detailed documentation.
Making the referral and prior authorization process. If the request is not approved please remember that you always have the option to purchase the medication at your own expense. Applied Behavior Analysis Request Form.
Prime number in PHP. ABA Therapy Request Form. The form should be printed filled out and then faxed or mailed to EHIM.
A number which is only divisible by 1 and itself is called prime number. What does it mean to get prior authorization. This form is for prospective concurrent and retrospective reviews.
See the Submitting Dental Service Authorization. Bariatric Surgery Request Form. A Prior Authorization is an approval for a specific drug or class of drug that is excluded from your benefit plan and does not allow coverage without a statement of medical necessity provided by the requesting physician.
If you have a referral then your provider gets prior authorization at the same time. _____ Member ID. If youre not required to get referrals you should know what services need prior authorization.
Here is the Program to list the first 15 prime numbers. Making sure the service needed is in-network and the requested procedure or treatment is necessary. Outpatient Rehab Therapy Request Form.