The EDI 835 and 837 transaction sets are an essential part of your process but you might not understand exactly what they do. 837 Q1 for professionals 837 Q2 for dental practices and 837 Q3 for institutions.
837 Health Care Claim Envelope Functional Group Header Gs Edi Blog Edi Blog
HIPAA 5010 837 transaction sets used are.
Edi transactions 837. This position will join a team of other EDI SMEs who are responsible for. 100-04 for further information on ASCA electronic billing requirements and enforcement reviews of health care professionals and suppliers. A CDPHP EDI analyst will contact the trading partner to provide user name password and all pertinent information needed enabling your organization to transfer files to CDPHP.
HIPAA 5010 837 transaction sets used are. Electronic Billing EDI Transactions. Receiving a fully completed ProviderGroup Access Information for 837 Transaction Set form available at the end of this document.
EDI is the automated transfer of data in a specific format following specific data. The EDI Health Care Claim Transaction set EDI 837 is used to submit health care claim billing information encounter information or both. The information in this section is intended for the use of health care providers clearinghouses and billing services that submit transactions to or receive transactions from Medicare fee-for-service contractors.
Refer to Chapter 24 Sections 90-906 of the. This CG also applies to ASC X12N 837P transactions that are being exchanged with Medicare by. EDI Healthcare Suite by Focused E-Commerce includes both claims management and remittance solutions and manages the EDI 835 and 837 transaction sets to ensure HIPAA compliance consistently.
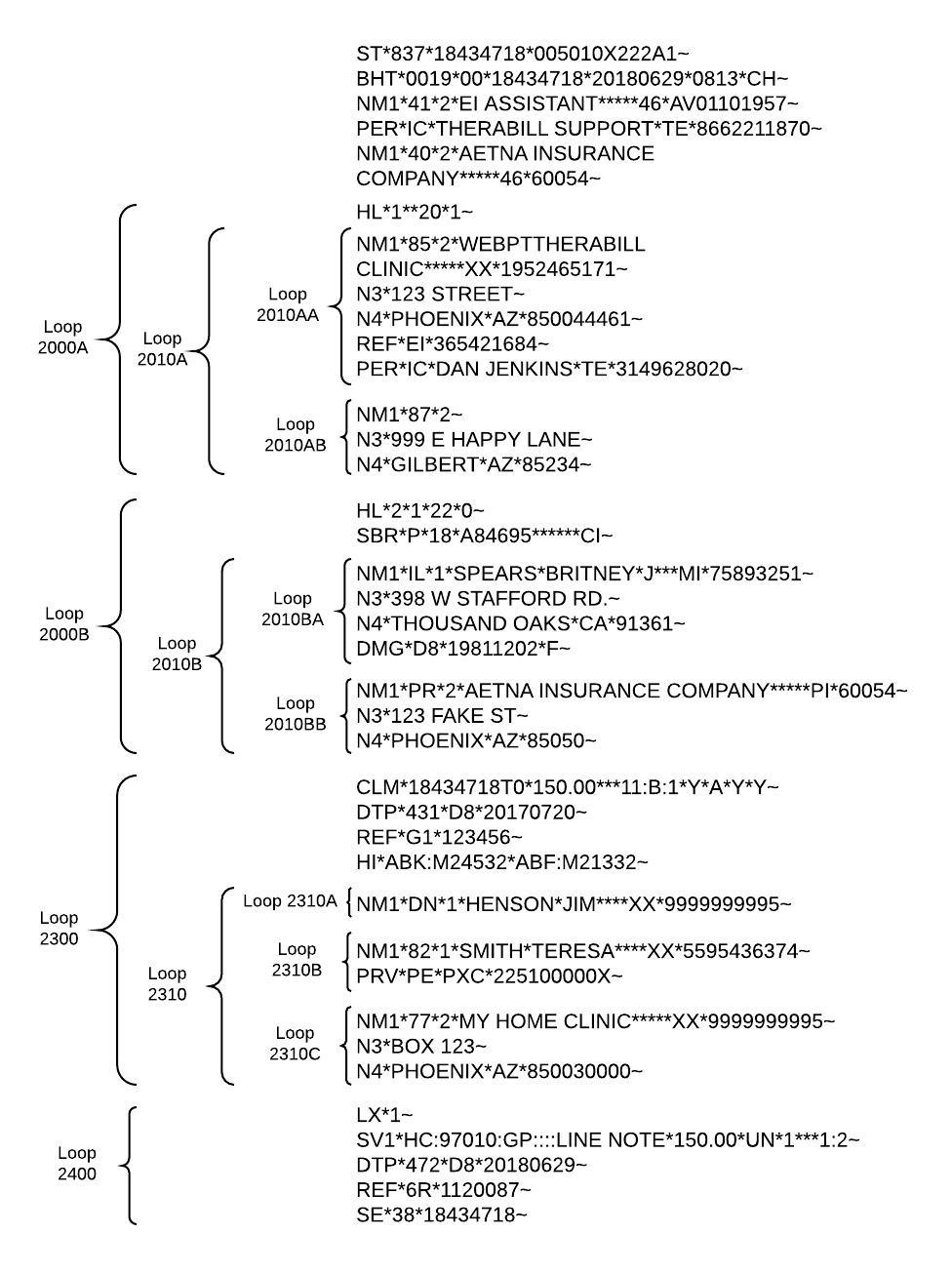
The 837-transaction set is the electronic submission of healthcare claim information. EDI Health Care Claim Transaction set 837 Used to submit health care claim billing information encounter information or both except for retail pharmacy claims see EDI Retail Pharmacy Claim Transaction. The EDI 837 Healthcare Claim transaction set and format have been specified by HIPAA 5010 standards for the electronic exchange of healthcare claim information.
Job Description This position is a Subject Matter Expert for the HIPAA 837 Claim Intake and Encounter EDI transactions. EDI addresses how Trading Partners exchange professional and institutional claims claim acknowledgments claim remittance advice claim status inquiry and responses and eligibility inquiry and responses electronically with Medicare. This Quick Reference Guide is part of a package of training materials to help you successfully.
EDI support furnished by Medicare contractors. Webpage and go to the left menu to select one of the ASCA options. It can be sent from providers of health care services to payers either directly or via intermediary billers and claims clearinghouses.
EMedNY Transaction Information CG June 22 2020 Page 3 of 65 Preface This Companion Guide to the v5010 ASC X12N Implementation Guides and associated errata adopted under HIPAA1 clarifies and specifies the data content when performing Electronic Data Interchange EDI with New York State Medicaid. 837 Transactions and Code Sets Electronic Transactions not only make good business sense. Healthcare service providers are required to be compliant with HIPAA EDI standards when submitting medical claims to payers in electronic format.
24 Supported Transactions The EIS supports the approved versions of the X12 and NCPDP Post Adjudicated Claims Data Reporting PACDR electronic health care transactions. Listed below are the supported inbound and outbound transactions. Providers sent the proper 837 transaction set to payers.
EDI 837 Transaction Set for Healthcare Claim Information The Healthcare Insurance Portability and Accountability Act better known as HIPAA was set in place in 1996 to protect patients private information as well as establish rules and requirements to stop fraud and waste in the industry. The EDI 837 transaction set is the format established to meet HIPAA requirements for the electronic submission of healthcare claim information. A description of the patient The patients condition for which treatment was provided.
It can be sent from providers of healthcare services to payers either directly or via intermediary billers and claims clearinghouses. 837 Q1 for professionals 837 Q2 for dental practices and 837 Q3 for institutions. They are also required by law.
The EDI 837 Healthcare Claim transaction set and format have been specified by HIPAA 5010 standards for the electronic exchange of healthcare claim information. Medicare Claims Processing Manual IOM Pub. The claim information included amounts to the following for a single care encounter between patient and provider.
Providers sent the proper 837 transaction set to payers.

