For the largest plan the Blue Cross and Blue Shield standard option biweekly rates for federal employees outside the Postal Service will be 11691 26715 and 28674 for self-only. Existing BCBS FEP Member Welcome to the 1 health insurance choice for federal employees retirees and their families.
 Fep Blue Cross Blue Shield 2018 Rates Rating Walls
Fep Blue Cross Blue Shield 2018 Rates Rating Walls
Get to know FEP Blue Focus Weve designed our newest coverage type with your needs in mind.

Blue cross blue shield federal employee program for retirees. You also have access to a registered pharmacist 247. About The Blue Cross and Blue Shield Service Benefit Plan FEP The Blue Cross and Blue Shield Service Benefit Plan also known as the Federal Employee Program FEP has been part of the Federal Employees Health Benefits FEHB Program since its inception in 1960. Medicare Supplement Insurance Plans are offered by Blue Cross and Blue Shield of Illinois a Division of Health Care Service Corporation a Mutual Legal Reserve Company an Independent Licensee of the Blue Cross and Blue Shield Association.
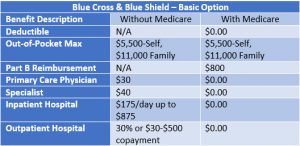
Federal Employee Program Blue Cross and Blue Shield of Montana This page may have documents that cant be read by screen reader software. As we mentioned before your health care benefits dont change after you retire if youre a member of the Blue Cross and Blue Shield Service benefit plan you get access to the great benefits you rely on now including worldwide coverage a large network of Preferred Providers Wellness rewards and discounts and you can still choose from one of our three plan options Standard option basic option and FEP blue focus. We help 54 million Federal employees retirees and their.
It covers roughly 55 million federal employees retirees and their families out of the more than 8 million people who receive their benefits through. For 60 years the Blue Cross and Blue Shield Service Benefit Plan also known as the Federal Employee Programor simply FEPhas provided health insurance to the federal employee workforce. Taking some small steps can add up to bigger.
Blue Cross and Blue Shield Federal Employee Program. We are proud to have been part of the Federal Employees Health Benefits FEHB Program since its inception in 1960. Government or Federal Medicare Program.
Today FEP covers over 55 million federal employees retirees and their families across the. Here are helpful Service Benefit Plan brochures claim forms reference guides and videos. 58460 likes 207 talking about this.
Call the National Information Center at 1-800-411-BLUE 2583 weekdays from 8 am. Prescription Coverage for Federal Employees and Retirees The Blue Cross and Blue Shield Service Benefit Plan has a variety of pharmacy programs to meet your prescription needs. If I decline Part B now and decide to take it later will I be subject to the Medicare Premium.
All benefits are subject to the definitions limitations and exclusions set forth in the federal brochure. The Blue Cross Blue Shield. 14 2020 PRNewswire -- Today the Blue Cross and Blue Shield Federal Employee Program FEP announced 2021.
You can get up to a 90-day supply for one copay. Before making a final decision please read the Plans federal brochure RI 71-017. 58459 likes 85 talking about this.
Not connected with or endorsed by the US. But if you decide to combine combine your your coverage coverage. Agency Benefits Officer - Federal Employee Program Blue Cross and Blue Shield of Illinois This page may have documents that cant be read by screen reader software.
Taking some small steps can add up to bigger. It covers roughly 55 million federal employees retirees and their families out of the more than 8 million people who receive their benefits through the FEHB Program. Learn how the Blue Cross and Blue Shield Service Benefit Plan and Medicare work.
For 60 years weve been covering federal employees and retirees. This is a summary of the features of the Blue Cross and Blue Shield Service Benefit Plan. To participate in the Mail Service Pharmacy Program complete the Mail Service Drug Prescription Form call CVS Caremark at 1-800-262-7890 or place an order through your MyBlue member account.
Service. Pages Businesses Finance Insurance Company Blue Cross and Blue Shield Federal Employee Program Videos Feeling stressed. For help with these documents please call 1-800-972-8382.
The Blue Cross and Blue Shield Service Benefit Plan is the number one choice of federal retirees in the Federal Employees Health Benefits Program. Blue Cross and Blue Shield Federal Employee Program. We help 54 million Federal employees retirees and their families live life well and with confidence.
I am covered under Federal Employees Health Benefits and pay for Blue CrossBlue Shield insurance. For help with these documents please call 1-800-634-3569.