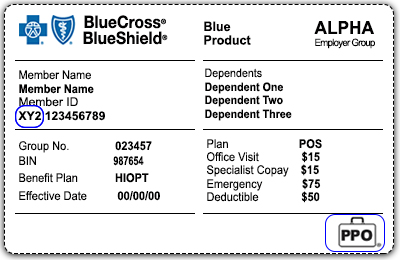
We suggest that you make copies of the ID card front and back and pass this key information on to your billing staff. Receive real-time responses to your eligibility requests through Availity or your preferred vendor portal.
Call BlueCard Eligibility at 800-676-BLUE 2583.
Bcbs blue card eligibility. If you select the Alternative Option you must submit relevant data or records showing a higher contribution percentage. Enter only the alpha prefix on the members ID number and your call will be routed to the members home plan. In the United States Puerto Rico and US.
You may be eligible to receive payment if you are an Individual Insured Group 1 and their employees or Self-Funded Account 2 and their employees that purchased or were enrolled in a Blue Cross or Blue Shield health insurance or administrative services plan during one of the two Settlement Class Periods. Verify eligibility and benefits. Verify Eligibility and Benefits.
Search for Doctors Hospitals and Dentists Blue Cross Blue Shield members can search for doctors hospitals and dentists. How to determine eligibility and coverage. If you are a Wellmark participating provider the easiest way to check eligibility and benefit information is through the Out-of-area Membership Search tool.
When conducting your search make sure to include the first three alpha characters on the Wellmark members ID card. Blue Cross Blue Shield Settlement co JND Legal Administration PO Box 91390 Seattle WA 98111. The members Plan then processes the claim and approves payment.
Members whose ID cards do not display a suitcase logo are excluded from receiving benefits through the BlueCard Program. 247 online access to account transactions and other useful resources help to ensure that your account information is available to you any time of the day or night. Submit the claim electronically to your local Blue Plan for faster processing.
Members whose ID cards display the blank suitcase logo are enrolled in a product other than PPO. Instructions for submitting your claim are on the claim form available here. BlueCard Eligibility and Benefits Call 1-800-676-2583 for eligibility and benefits prior to services being rendered.
Call Blue Card Eligibility 800-676-BLUE 2583. Number on the ID card. BCBSMT electronically routes the claim to the members BCBS Plan.
If you are an out-of-state provider and participate with another BCBS Plan you can access eligibility and benefits information through your local BCBS Plans website. Otherwise the Default Option will be used. Outside the United States.
Submit an electronic eligibility and benefits inquiry 270 transaction to BCBSIL via the Availity Provider Portal or your preferred web vendor. To verify dental eligibility and benefits. As a current member you can access your benefits and services from your local Blue Cross Blue.
ID cards are for identification purposes only. The members ID card or the acknowledgement letter from Blue Cross Blue Shield of Michigan shows that the member is enrolled in a plan. Its easy to verify eligibility and find out about the members benefits.
Call the Blue Card Eligibility line at 800-676-BLUE 2583. For out-of-state Blue Cross and Blue Shield members call the BlueCard Eligibility Line at 800-676-BLUE 2583 for eligibility and benefit verifications. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States.
57 rijen 800-676-2583 Blue Card Eligibility 877-228-7268 Blue Card Eligibility Out of. These members are also eligible for BlueCard processing. 4 Submit the claim to BCBSMT with the alpha prefix.
You can also call 800-676-BLUE. MyBlue offers online tools resources and services for Blue Cross Blue Shield of Arizona Members contracted brokersconsultants healthcare professionals and group benefit administrators. You should always verify patient eligibility by calling 1800676BLUE 2583 Introduction.
They do not guarantee eligibility or payment of your claim. Check benefits and eligibility by either using your local Blue Plans electronic capabilities or by calling 1800676BLUE 2583. Check Benefits and Eligibility.
The Program BlueCard Our commitment to you BlueSM providers just like you serve nearly 100 million Blue members nationwide including almost. You can check whether the Home Plan requires prior authorization by using the BlueCard Precertification tool. A BlueCard Eligibility Representative will connect you to the appropriate plan where eligibility and benefits can be obtained.
To check claim status contact your local Blue Plan. Enter only the three-character prefix on the members ID number and your call will be routed to the members home plan. Provide the three-character prefix as it is listed on the members identification ID card.
Check benefits and eligibility for BlueCard members by calling 800-676-BLUE 2583 and providing the prefix or by using My Insurance Manager SM. Learn more about BlueCard For Federal Employee Program FEP members eligibility and benefits can be obtained by calling 800-972-8382. Call 1-800-676-BLUE 2583 Use web-DENIS.
Receive real-time responses to your eligibility requests by logging on to our Secure Provider Portal and clicking on BlueExchange. 3 Call BlueCard Eligibility at 1800676BLUE 2583 to verify membership and coverage. Youll need the prefix from the patients member ID card.