Most health insurers including Medicaid and Medicare typically only cover genetic testing when youre showing signs or symptoms of an illness that would be better understood through diagnostic testing. Genetic testing and counseling are covered when Medicare coverage criteria are met.
 Perceived Or Experienced Coercion To Undertake Genetic Testing Download Table
Perceived Or Experienced Coercion To Undertake Genetic Testing Download Table
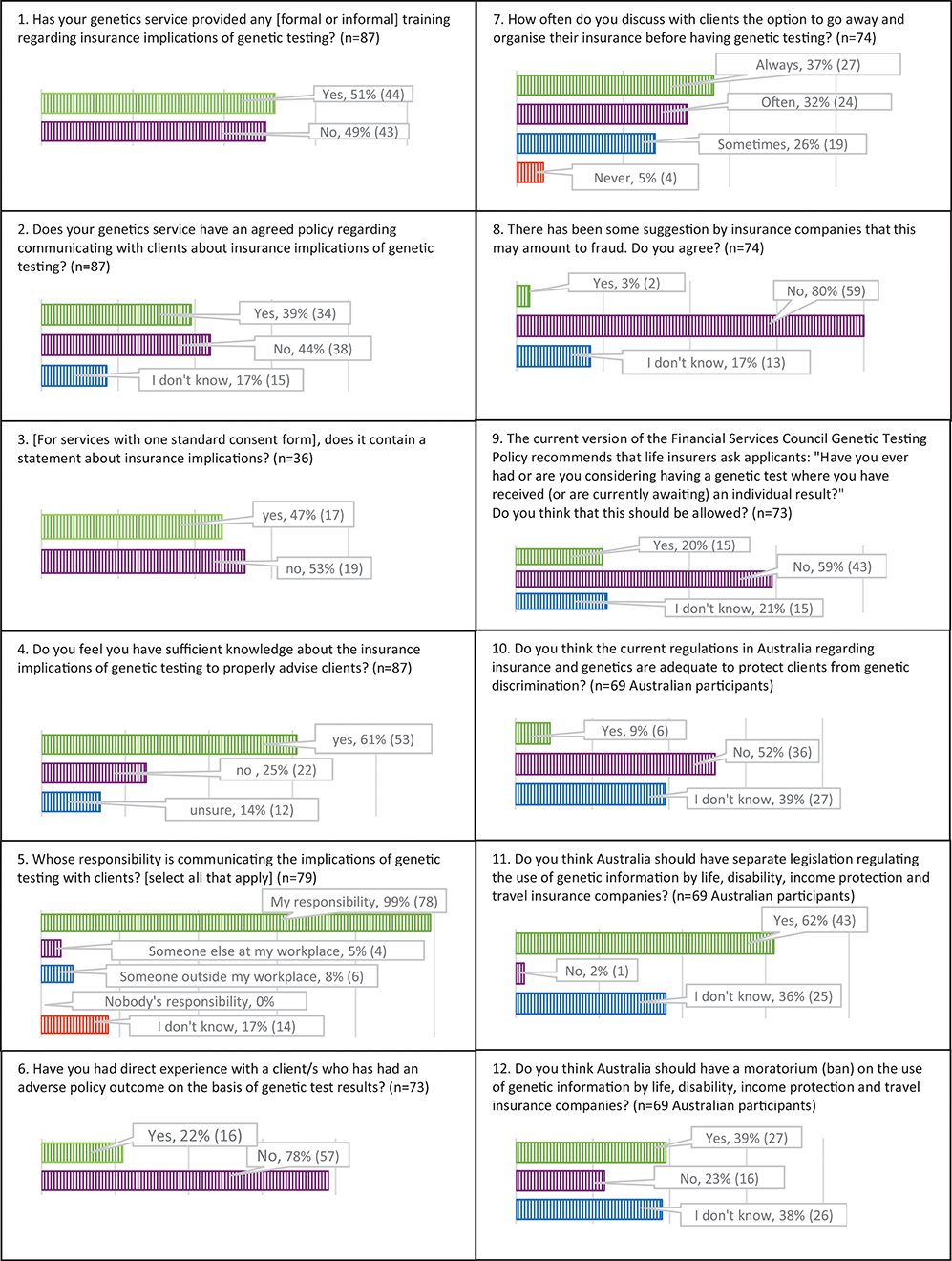
The insured worry about discrimination.

Is genetic testing covered by insurance. Different states have other laws related to. Approximately one-third of insurers had at least one genetic testing policy. Health insurance providers have different policies about which tests are covered however.
Some plans may also offer coverage for routine dental hearing and vision care as well as some other benefits. Most health insurance plans will cover the cost of genetic testing when recommended by a physician. Many Medicare Advantage plans may offer prescription drug coverage.
The law however does not prevent people from discrimination related to life insurance or long-term care or disability insurance. You or your doctor may be required to submit documentation proving that you have a certain diagnosis or have experienced difficulty finding the. In many cases health insurance plans will cover the costs of genetic testing when it is recommended by a persons doctor.
We documented the number of policies tests mentioned coverage determination and policy effective dates. This means that health insurance companies cannot use the results of a direct-to-consumer genetic test or any other genetic test to deny coverage or require you to pay higher premiums. Initial genetic testing for mutations on the BRCA1 and BRCA2 genes which typically serve as tumor suppressors costs roughly 4000 when not covered by insurance according to Myriad Genetics.
Screening services such as predictive and presymptomatic genetic tests and services are those used to detect an -. Coverage for preimplantation genetic testing Starting July 1 2021 preimplantation genetic testing PGT will be covered as a standard benefit for eligible UnitedHealthcare commercial plan members when they or their partners are carriers for a specific genetic disorder. Therefore ASCO strongly encourages you to verify with the patients insurer to understand what type of services will be covered.
The gene is out of the bottle Genetic testing threatens the insurance industry. However all coverage and reimbursement is subject to Medicare Medicaid and third-party payer benefit plans. According to the ACLI if an insurer asks about genetic tests on a life insurance application it would only be interested in an at-home test if your results came back with a recommendation that you.
The federal Genetic Information Nondiscrimination Act does prohibit insurers. A licensed insurance agent can help you compare available Medicare Advantage plans in your area. Coverage and Reimbursement of Genetic Tests For patients to have full access to the benefits of genetic testing payers such as insurance companies and Medicare need systematic ways of evaluating genetic tests for reimbursement.
Insurers worry about adverse selection. Insurance Coverage for Genetic Testing Insurance coverage for genetic testing may vary depending on your insurance plan and personal history. A person interested in submitting the costs of testing may wish to contact his or her insurance company beforehand to ask about coverage.
In general long-term-care insurers can indeed use genetic test results when they decide whether to offer you coverage. However GINA does not apply when an employer has fewer than 15 employees. It also prevents people from employment discrimination based on genetic testing.
If your genetic test is covered by Original Medicare it will also be covered by a Medicare Advantage plan. Some insurers have opted to cover genetic tests in cases where the patient is deemed high risk a common case is the breast cancer risk test which insurers tend to pay for only when the patient.