Family size adjustments HUD applies to the income limits and 4 determining income limit levels applicable to Californias moderate-income households defined by law as household income not exceeding 120 percent of county area median income. Their maximum contribution would be 1485 and their benchmark plan would be 644.
 Covered California Income Limits Explained
Covered California Income Limits Explained
The unshaded columns are associated with Covered California eligibility ranges.

Covered california income limits. Medi-Cal Eligibility and Covered California - Frequently Asked Questions. In certain limited circumstances however they are eligible for the federal. Under the new 2021 income limits.
How to Estimate Your Income. Below you will find the most frequently asked questions for current and potential Medi-Cal coverage recipients. April 15 2016 OutreachandSalescoveredcagov or Low to help determine if you qualify Income Guidelines use through October 2016 You may be eligible for Medi-Cal -Income Health Plan.
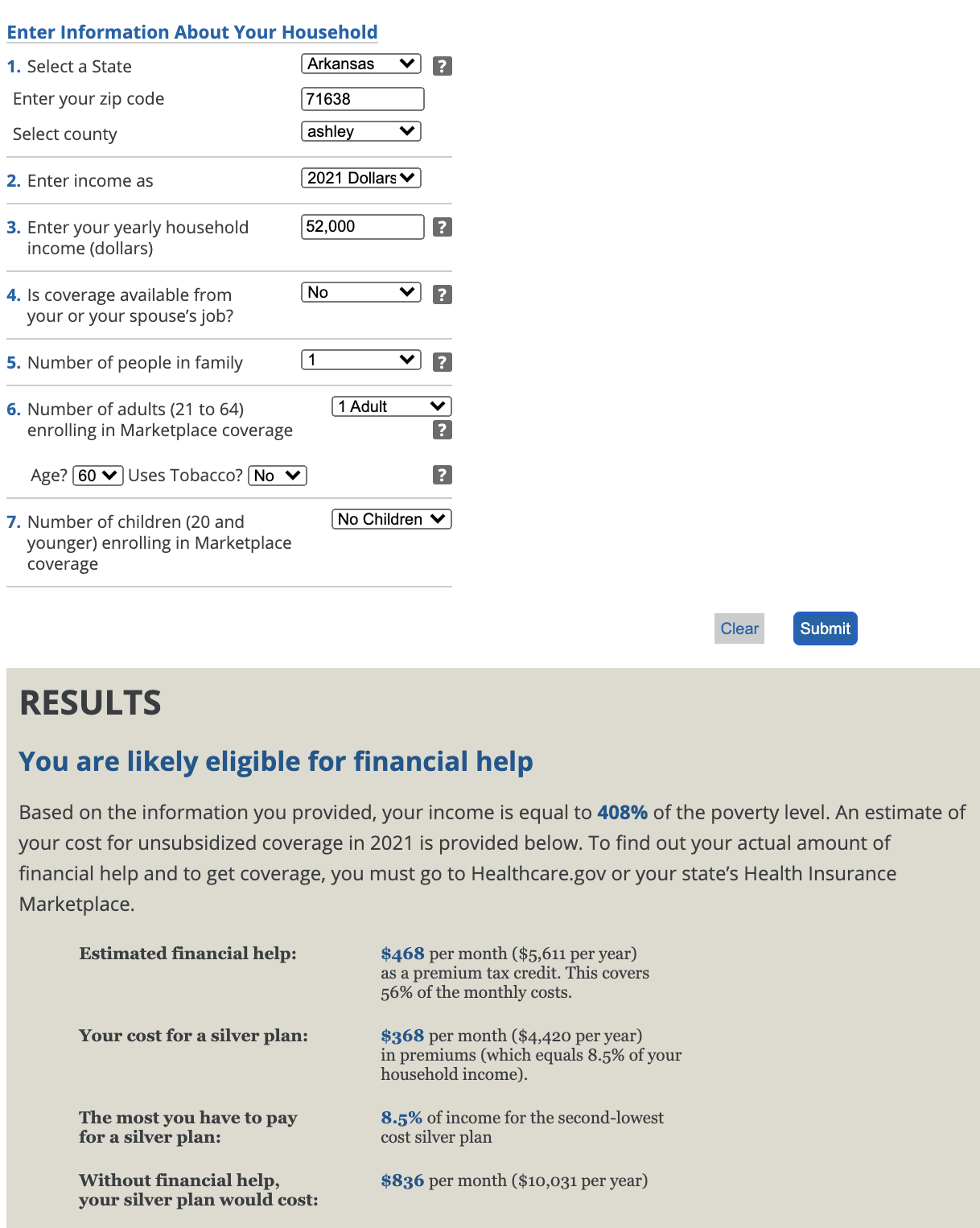
For people with a household income that is below 400 of the Federal Poverty Level FPL Covered Ca may qualify them to receive financial assistance also called a Subsidy which reduces their premium. You can start by using your adjusted. Back to Medi-Cal Eligibility.
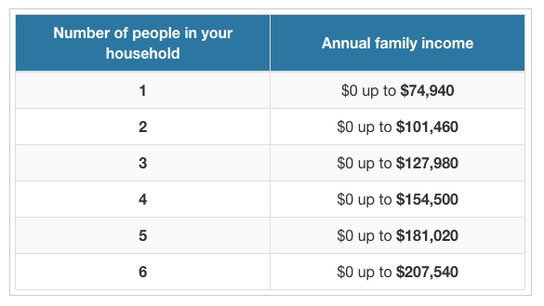
To qualify for government subsidies you must purchase your coverage through Covered California and your annual gross income cannot be more than 400 percent of the FPL. When you calculate your income youll need to include the incomes of you your spouse and anyone you claim as a dependent when you file taxes. You may qualify for no-cost or low-cost Medi-Cal and may be able to switch plans if you currently.
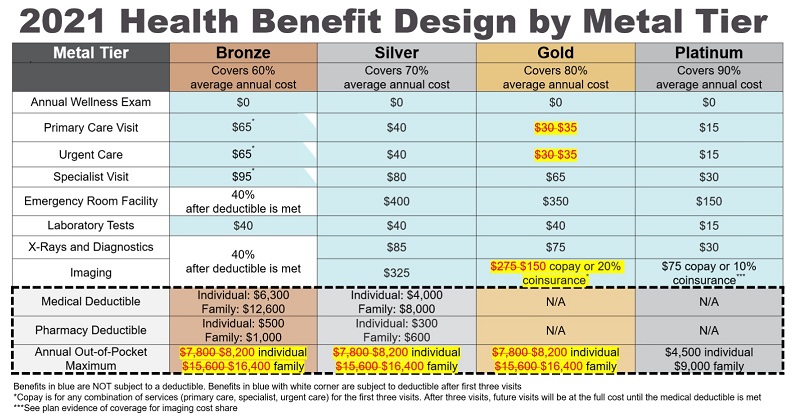
For Bronze and Silver there are no other benefit changes for next year. Covered california california health benefit exchange and the covered california logo are registered trademarks or service marks of covered california in the united states. Bronze Silver and Gold The out-of-pocket maximum is going up from 7800 to 8200 on the Bronze Silver and Gold Plans.
Alimony only if divorce or separation finalized before Jan. Individuals with income at or below 138 of the federal poverty level are generally eligible for Medi-Cal Californias Medicaid program. This program is meant to limit how much a Californian will pay for their health insurance premium as a percentage of their income according to Covered California.
How do I know if I qualify for a subsidy. If you make 601. If you do you are not eligible for a subsidy.
Covered California Programs Medi-Cal Programs Percentage of income paid for premiums based on household FPL Based on second-lowest-cost Silver plan Household FPL Percentage Percent of Income 0-150 FPL 0 household income 150-200 FPL 0-2 household income 200-250 FPL 2-4 household income 250-300 FPL 4-6 household income 300-400 FPL 6-85. Excluded untaxed foreign Income. Covered California Outreach and Sales Division Updated.
Pandemic Unemploment Compensation 300week Social Security. Any financial help you get is based on what you expect your household income will be for the coverage year not last years income. Or Medi-Cal Beneficiary Medi-Cal income levels have.
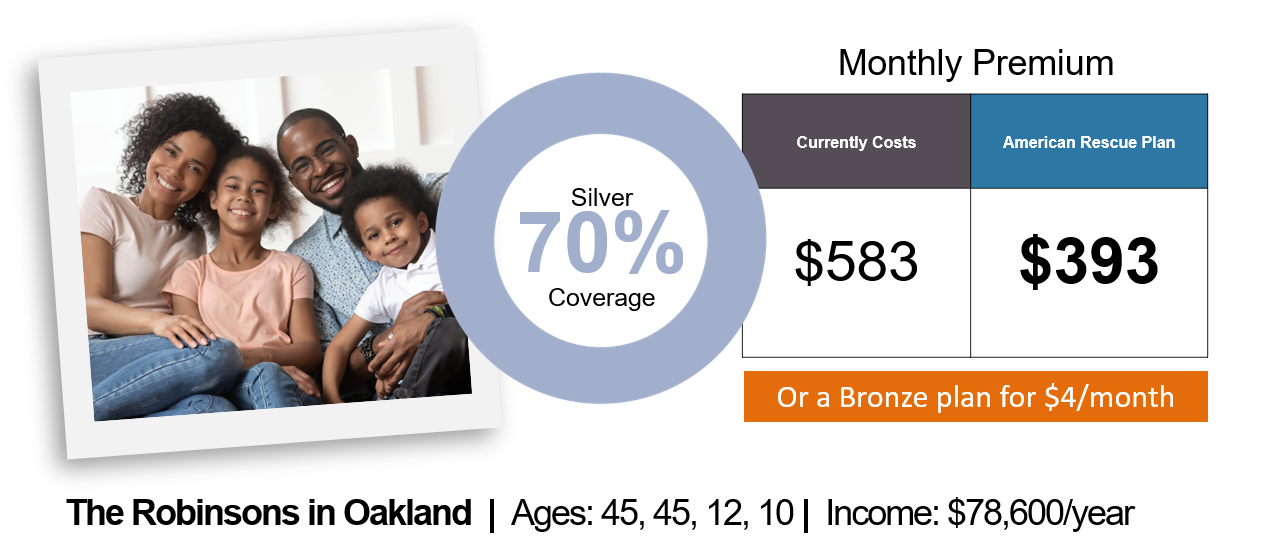
The income thresholds to qualify for the additional help from the state are 74940 for an individual 101460 for a couple and 154500 for. That means you can earn no more than 134960. A 30-year-old couple with a household income of 100000.
In order to be eligible for assistance through Covered California you must meet an income requirement. California State Subsidy 0138 FPL over 200600 FPL Federal Tax Credit 100400 FPL Enhanced Silver Plans 100250 FPL. Social Security Disability Income SSDI Retirement or pension.
In order to qualify for federal tax credits or a subsidy in California you must make between 0-600 of the FPL. 300 - 400 FPL. Covered California rates are going up 06 on average and the plan benefits are not changing very much.
This means that a family of four with an annual income of around 150000 per year may be eligible for subsidies. This site is not maintained by or affiliated with covered california and covered california bears no. Because their benchmark plan costs less than their maximum contribution there is no State credit to make up the difference.
Whether you qualify for financial assistance depends on your household income and. So lets say youre a family of six. These are the repayment limits for the state subsidy received in 2020.
Repayment is suspended for any extra premiums you received in tax year 2020 because of the American Rescue Plan which passed in March 2021. This web site is owned and operated by health for california which is solely responsible for its content. Covered California uses FPL limits from the prior year to determine eligibility for its programs as required by regulation.
If you do not find an answer to your question please contact your local county office from our County Listings page or email us.