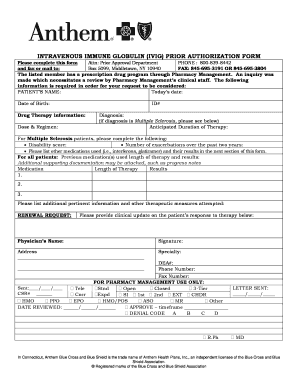
Form 8962 Department of the Treasury Internal Revenue Service Premium Tax Credit PTC Attach to Form 1040 1040-SR or 1040-NR. You need to use 8962 Form to reconcile your estimated and precise income for the yr.
 Printable Tax Form 8962 Fill Out And Sign Printable Pdf Template Signnow
Printable Tax Form 8962 Fill Out And Sign Printable Pdf Template Signnow
The IRS uses Form 8962 to reconcile the tax credit the well being plan obtained based mostly on the individuals estimated revenue with the amount of his or her actual earnings as reported on their federal tax return.

What is irs form 8962. You only need to complete Form 8962 if you received advance payments of premium tax credits for health insurance premiums paid. The 8962 form will be e-filed along with your completed tax return to the IRS. Form 8962 is used to calculate the amount of your premium tax credit PTC and reconcile any advance premium tax credit APTC taken.
Usually if the tax deadline is near any tax credit and refund may. Form 8962 Premium Tax Credit is required when someone on your tax return had health insurance in 2020 through Healthcaregov or a state marketplace and took the Advance Premium Tax Credit to lower their monthly premium. The deadline for the IRS Form 8962 for the year 2020 is 15 April 2020.
Who Can Use Form 8962. Some tax professionals call it the IRS health insurance form 8962 since the form kickstarts the process for receiving a valuable tax credit for households with little to moderate income levels. The IRS is requesting Form 8962 for 2020.
If you did not e-file your return with the Form 8962 for the Premium Tax Credit the IRS might send you a letter asking for this information. Multiply the difference by 100 then drop any numbers after the decimal point. Your social security number.
Be sure to check if the letter references tax year 2017 2016 or 2015. Well help you create or correct the form in TurboTax. Form 8962 Premium Tax Credit PTC is the form you will need to report your household Modified AGI MAGI your Federal Poverty Level amount your familys health insurance premium exemptions and the cost assistance you received.
36B premium tax credits to report for the 2020 tax year are not required to file Form 8962 Premium Tax Credit or report an excess advance premium tax credit APTC repayment on their 2020 Form 1040 US. The purpose of Form 8962 is to allow filers to calculate their Premium Tax Credit PTC amount and to reconcile that amount with any advance payments of the Premium Tax Credit APTC that have been made for the filer throughout the year. Go to wwwirsgovForm8962 for instructions and the latest information.
Name shown on your return. Receiving too much in advanced premium tax credits could result in you owing money to the IRS when you file your tax return26 мая 2020 г. June 7 2019 354 PM Turbo Tax can help you complete a form 8962 if you have received a letter from the IRS asking for an update.
Form 8962 is an essential tax form that not only helps relieve the pressure of your return but also makes affordable health insurance through the marketplace viable to everyone. What Is form 8962. 8962 IRS Form 8962 A premium tax credit or PTC is a type of refundable tax credit that allows low income and middle income individuals and families cover the premiums of health insurance bought in the Health Insurance Marketplace.
About Form 8962 Premium Tax Credit Internal Revenue Service. Form 8962 is used either 1 to reconcile a premium tax credit advanced payment toward the cost of a health insurance premium or 2 to claim a premium tax credit. Form 8962 is used to calculate the amount of premium tax credit youre eligible to claim if you paid premiums for health insurance purchased through the Health Insurance Marketplace.
Who must file IRS Form 8962. Not everyone can file Form 8962 and claim the Premium Tax Credit. Below we do a walkthrough of filling out the PTC form and we simplify the terms found within.
The IRS announced on Friday that taxpayers who may have had excess Sec. The form in question is the IRS 8962 form. This premium tax credit is immensely useful.
For example if the difference was 18545565 you would enter 185 on line 5 of Form 8962. Its specifically designed to cover health insurance and reconcile the credit given to such people through Health Insurance Marketplace. Individual Income Tax Return or Form 1040-SR US.
If you have enrolled in a health insurance plan through the. The 5-Part Breakdown of Form 8962. Each individual has to file appropriate tax forms with the IRS to report certain financial details.
The 8962 form also known as Premium Tax Credit is a document used by individuals or families whose income is below average. Such documents can be used for reporting income earned amount of tax paid or to prother data required.