The Cal MediConnect program launched in 2014 and was ultimately implemented in seven counties. As a SCFHP Cal MediConnect member you have access to classes and programs to help you manage your health.
 Cal Mediconnect Santa Clara Family Health Plan
Cal Mediconnect Santa Clara Family Health Plan
Monthly gym membership with pre-authorization from plan nurse or case manager.
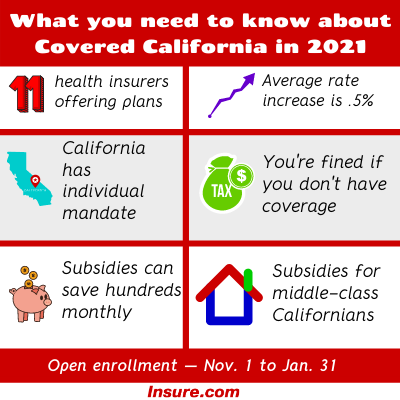
Cal mediconnect program. Your SilverSneakers benefit starts as soon as you are enrolled in LA. California Medi-Connect Program. Sometimes a Cal MediConnect plan is called a managed care plan Your doctor will work with the Cal MediConnect plan to provide you services.
This voluntary program consolidates the overlapping properties of. April 4 2013. To 8 pm Monday through Friday.
CareMore accepts Anthem Blue Cross Medicare-Medicaid Plan MMP as part of this program. Get the most from your Medicare and Medi-Cal benefits. Your call will be returned within the next business day.
Health Risk Assessments in the Cal MediConnect Program What is Cal MediConnect. In addition to your current Medi-Cal and Medicare benefits CommuniCare Advantage Cal MediConnect Plan includes. The Cal MediConnect Program is an important innovation in the nations health care system to help out the nations most low income individuals those who qualify for both Medicare and Medi-Cal dual eligible members.
Cal MediConnect is a program that integrates medical care long-term care mental health and substance use programs and social services under a coordinated care plan for people who are dually eligible for Medicare and Medi-Cal. Cares Cal MediConnect members have access to member services representatives who speak their language. For more information on Health Nets Cal MediConnect plan please call.
To 800 pm Hours are from 8 am. Jenna MacRae Attorney Registered HICAP Counselor Elder Law Advocacy. With Cal MediConnect Health Net can help you.
Some of Our Services Include. Health Net Cal MediConnect Plan is a program to serve people that are eligible for both Medicare and Medi-Cal. Health Education services are designed to support our members in living healthier lives.
A Cal MediConnect plan puts a coordinated organization of doctors hospitals pharmacies and providers at your fingertips with the help of an experienced Care Navigator. Health Insurance Counseling and Advocacy Program HICAP a program of Elder Law Advocacy. Cal MediConnect is an all-in-one health plan that covers medical prescription drugs medicines and long-term services and supports.
SilverSneakers Program SilverSneakers is a new no-cost fitness benefit for LA. Overview of Medi-Cal. The program is being implemented in seven counties.
After you join a plan you must get your services from the plans providers. You may need approval for some services. Chronic disease management for asthma diabetes high blood pressure etc.
The Cal MediConnect CMC program is a voluntary demonstration operated by the Department of Health Care Services DHCS in collaboration with the Centers for Medicare and Medicaid Services CMS to provide better coordinated care for beneficiaries eligible for both Medicare and Medicaid also known as duals. Cal MediConnect is the name of Californias Demonstration. Hospital inpatient outpatient physician services and custodial level long.
Los Angeles Orange Riverside San Bernardino San Diego San Mateo and Santa Clara. Each Cal MediConnect plan has its own group of providers. Your care team will.
An Overview of the Coordinated. The Cal MediConnect Program is an important innovation in the nations health care system to help those who qualify for both Medicare and Medi-Cal dual eligible members. How to Choose a Plan.
This exciting program gives you a free basic gym membership at more than 15000 fitness center locations across the country. This group is the plans network of providers. The Care Navigator coordinates all of your providers and services to make sure you get the care you need and is available to answer your questions and refer you to any community resources you may need.
The goal of the Cal MediConnect program is to help members avoid unnecessary hospitalizations and placement in long-term care facilities and to lead more independent lives in the comfort and familiarity of their own homes and communities. Worldwide emergency services excludes transportation back to the US. What is Cal MediConnect.
Care Initiative in. All classes and programs are provided at no cost to SCFHP Cal MediConnect members. After hours on weekends and on holidays you can leave a message.
He Cal MediConnect program aims to coordinate medical behavioral health long-ter m institutional and home- and community-based services through a single health plan for beneficiaries dually eligible for both Medicare and Medi-Cal. StateFederal program for low-income individuals including families with children youth in foster care seniors and people with disabilities. San Bernardino County.
Care Cal MediConnect members. Cal MediConnect is a major component of the Coordinated Care Initiative CCI which aims to integrate and coordinate the delivery of health behavioral and long-term care LTC services for duals seniors and people with disabilities who have Medi-Cal. This voluntary program was developed by the California Department of Health Care Services in conjunction with the Centers for Medicare Medicaid Services.