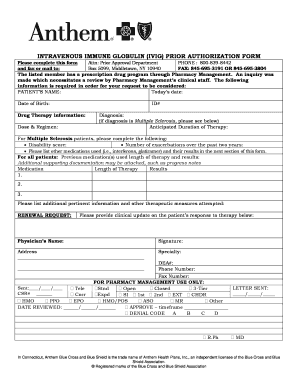
Make sure you include your office telephone and fax numbers. Non-Formulary Exception and Quantity Limit Exception PDF 129 KB Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB.
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Medicaid only BCCHP and MMAI Medicaid Service Authorization Dispute Resolution Request Form.
Blue cross blue shield of az prior authorization form. Urgentemergency admissions do not require prior authorization. Call 1-888-233-8158 from 800 am. Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members.
Medicaid only BCCHP and MMAI. GENERAL INFORMATION Patient Name Request Type please check one Prior Authorization Step Therapy Exception Request for Quantity Limit Exception City Appeal Mandatory Generic Exception Request for Non-Formulary Exception. The protection of your privacy will be.
BlueCard appeal submission - For out-of-area BlueCard members appealing the home Blue plan. We review them to ensure they are medically necessary. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required.
The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Blue Cross PPO Request for Preauthorization Form PDF Medicare Plus Blue PPO. To find out if you qualify for transition of care BCBSTX may need to request medical information from your current providers.
During this time you can still find all forms and guides on our legacy site. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Blue Advantage Physician Drug Authorization Request Form.
You will be notified by fax if the request is approved. You can submit the form by mail or fax to BCBSTX. AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out.
Member authorization is embedded in the form for providers submitting on a members behalf section C. Find authorization and referral forms. You will be going to a new website operated on behalf of the Blue Cross and Blue Shield Service Benefit Plan by a third party.
The following guidelines apply to Anthem Blue Cross and Blue Shield Anthem products issued and delivered by Anthem in New Hampshire. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Provider Forms Guides.
Form Title Networks Expedited Pre-service Clinical Appeal Form. This is called prior approval precertification or preauthorization. Prior Approval Pharmacy Forms.
For information on precertification requirements for those members of National. BlueRx Drug Prior Authorization. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Medicaid Claims Inquiry or Dispute Request Form. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
If you do not obtain prior approval there may be a reduction or denial of your benefit. Medicare Plus Blue PPO non-Michigan Skilled Nursing Facility Acute Rehabilitation Facility Fax Assessment Form PDF Medicare Plus Blue PPO LTACH Fax Assessment Form PDF Medicare Plus Blue PPO Acute Inpatient Fax Assessment Form PDF. Certain medical services and treatments need approval before you receive care.
View our individual plans page for additional appeal forms. Blue Advantage Drug Coverage Determination Formulary or Tier Exception Drug Authorization Forms Quantity Limit Drug Authorization Forms and Step Therapy Drug Authorization Forms. To 900 pm Eastern Monday through Friday.
Blue Advantage Drug Prior Authorization. We are currently in the process of enhancing this forms library. If you are approved for transition of care in-network benefits may be available for up to 90 days after your provider leaves the network.
Download a form from the Forms Resources section of the Evicore website and fax it to 1-888-693-3210. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. If you need preauthorization contact eviCore in one of three ways.
When completing a prior authorization form be sure to supply all requested information. 17 rijen Out-of-Network Enrollee Notification Form for Non-Regulated Business Use this. Some services require prior authorization preauthorization before they are performed.
Authorized Representative Designation Form. Anthem Blue Cross and Blue Shield in New Hampshire. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review.
Fax completed forms to FutureScripts at 1-888-671-5285 for review. Fill out a transition of care form.