Use the Pre-CertPre-auth Router out-of-area members to view the applicable Blue Plans medical policy or general pre-certificationprior authorization information. The Pre-service Review for BlueCard Members tool for out-of-area members or by calling 1-800-676-BLUE.
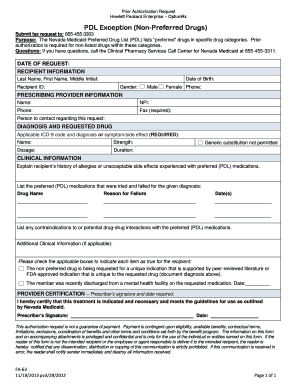
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
EviCore is an independent company that provides specialty medical benefits management for BCBSNM.
Blue cross blue shield pre authorization. Information for Blue Cross and Blue Shield of Illinois BCBSIL members is found on our member site. To verify coverage or benefits or determine prior authorization requirements for a participant call 1-800-442-2376 or send an electronic inquiry through your established connection with your local Blue plan. Prior authorization or pre-authorization is a review prior to the time a specified procedure is scheduled.
Advertentie Compare 50 Global Health Insurance Plans for Expats living abroad. Pre-authorization Prior authorization. Prior authorization sometimes called pre-certification is how Blue Cross and Blue Shield of Minnesota makes sure the treatment your doctor prescribes is medically necessary and helps ensure you are getting proper care.
You or the patient would need to contact Integrated Health the Arkansas Blue Cross and Blue Shield pre-notification vender by calling 1-800-451-7302. For some services listed in our medical policies we require prior authorization. When prior authorization is required you can contact us to make this request.
We use established clinical guidelines to confirm medical necessity when your health plan requires prior authorization. We review them to ensure they are medically necessary. This information is NOT to be relied upon as prior authorization for health care services and is NOT A GUARANTEE OF PAYMENT.
The notification timeframes for calling Blue Cross and Blue Shield and benefit reductions are described below under the provision entitled Benefit Reductions for Failure to Obtain Prior Authorization or Notify. Home health services and short-term rehabilitation When our guidelines are followed we automatically approve initial authorization requests for these services for our managed care members. Get a Free Quote.
BUFFALO In 2017 the regions leading health plan BlueCross BlueShield of Western New York has announced significant changes that will allow members more efficient access to care as directed by their physicians and other health care providers without having to wait for approval from the health plan a process known as Preauthorization. Provider Preauthorization and Precertification Requirements - Blue Cross PPO and Medicare Plus Blue SM PPO PDF Northwood DMEPOS Management Program FAQ PDF Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts. Certain medical services and treatments need approval before you receive care.
To verify coverage or benefits or determine pre-certification or pre-authorization requirements for a particular member call 1-18006762583 or send an electronic inquiry through your established connection with your local Blue Plan. You are responsible for making sure your prior authorization requirements are met. Get a Free Quote.
Advertentie Compare 50 Global Health Insurance Plans for Expats living abroad. Sometimes a plan may require the member to request prior authorization for services. A preauthorization is the process where we review the requested service or drug to see if it is medically necessary and covered under the members health plan.
Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Usually the provider is responsible for requesting prior authorization before performing a service if the member is seeing an in-network provider. Blue Cross and Blue Shield of New Mexico BCBSNM has contracted with eviCore Health TM eviCore to provide certain utilization management preauthorization services for Medicare Members.
This information is not to be relied upon as pre-authorization or pre-certification for health care services and is not a guarantee of payment. Outpatient Prior Authorization CPT Code List 072 Prior Authorization Quick Tips. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required.
If you do not obtain prior approval there may. Not all services and drugs need preauthorization. Services requiring preauthorization through eviCore are outlined below.
If pre-certificationprior authorization is required submit an electronic request 278 transaction through Availity or your preferred web vendor portal. Preauthorization also called prior authorization or prior approval are a pre-service medical necessity review. Prior review prior plan approval prior authorization prospective review or certification is the process Blue Cross NC uses to review the provision of certain behavioral health medical services and medications against health care management guidelines prior to the services being provided.
This is called prior approval precertification or preauthorization.