Just fill out this appoint a representative form and mail to the address below. If you need assistance with your Availity account call the Availity Client Services team at 1-800-AVAILITY.
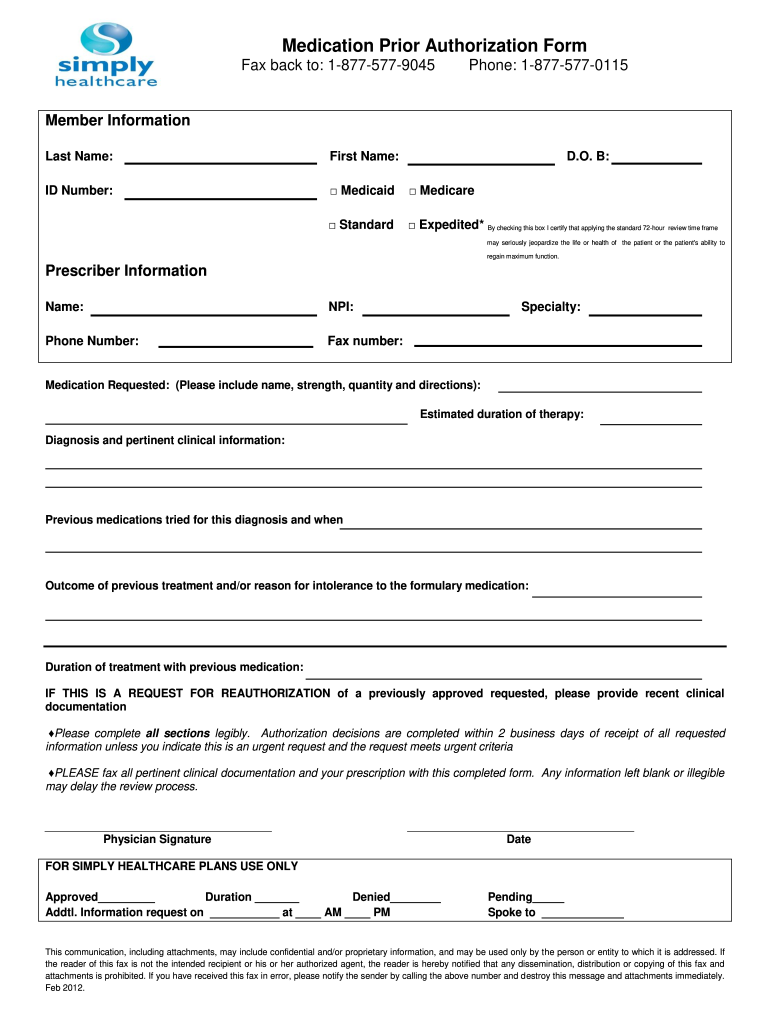 Simply Healthcare Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
Simply Healthcare Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
Call us at 855-442-9900.
Bright health medicare advantage prior authorization form. How to submit an authorization request. If you have any questions regarding this form andor would like more information about Bright Healths. The Medicare Prior Rx Authorization Form or Drug Determination Request Form is used in situations where a patients prescription is denied at the pharmacy.
Bright Health PO Box 853959 Richardson TX 75085-3959. To ensure our patients receive quality and timely care please complete this form in its entirety and submit with appropriate supporting clinical documentation. Arkansas Blue Cross EmployeesDependentsRetirees- Designation for Authorized Appeal Representative Form pdf.
Once a patient or their physician receives a written denial coverage determination they should submit a coverage determination request form asking for the drug to be covered. Per prior authorization bill HB19-1211 or CRS. If you need to make a change to your SelectHealth plan theres a form for that.
Meridian Idaho 83642 208-345-4550 Mailing Address. Fax the request form to 8886476152. Last Updated March 3 2021.
SECTION 3 SERVICE INFORMATION CPT codes are used to determine the type of services requested. Text maskedTwoFactorSMS Email maskedTwoFactorEmail Use my authenticator app. To request prior authorization please submit your request online or by phone.
As a provider outside of Michigan who is not contracted with us you should submit Medicare authorization requests via fax using the proper prior authorization form. Individual and Family Plans Call. Complete your fax cover sheet included on next page STEP 2.
This includes but not limited to completing this form in its entirety and submitting with appropriate. All Medicare authorization requests can be submitted using our general authorization form. For additional security we need to verify your identity before you can sign in to the account.
Provider Request for Commercial Prescription Drug Coverage Determination. Provider Request for Medicare Prescription Drug Coverage Determination. Providers can view the current status of a submitted prior-authorization at any time.
Medicare Advantage Prior Authorization Request Please do not use for Commercial Products 2016 by Blue Cross of Idaho an independent licensee of the Blue Cross and Blue Shield Association 3000 E. The appointment lasts up to a year unless you cancel it first. You have the right to request an organization determination if you want us to provide or pay for an item or service you believe should be covered.
Then select the Prior Authorization and Notification tool on your Link dashboard. This reduces back and forth between provider and payer. Hospice Pharmacy Authorization Request Form.
Use the Prior Authorization and Notification tool on Link. Create Date February 28 2020. Prior Authorization Step Therapy.
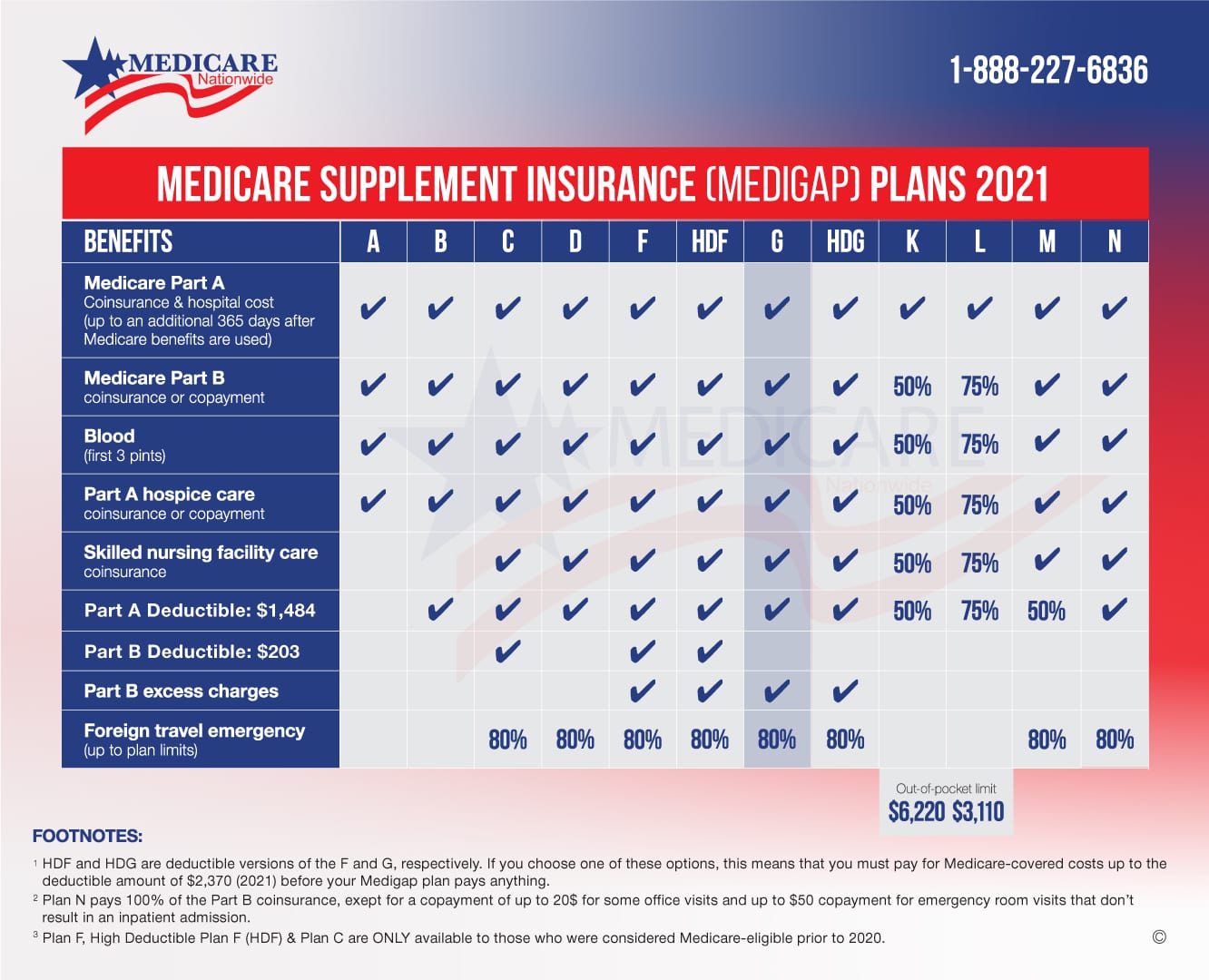
Medicare Advantage Prior Authorization Request Prominence Health Plan. Authorization of these services assumes that you will bill with codes billable under the current Medicare Fee Schedule. Prior Authorization Request Form Supporting Clinical Documents Remember to provide the required information to ensure our members receive quality and timely care.
CONFIDENTIAL MEDICARE ADVANTAGE PRIOR AUTHORIZATION REQUEST FORM BEHAVIORAL HEALTH REQUEST Required Information. Medicare Advantage Prior Authorization Request. Formulary Prior Authorization Lists.
File Size 12198 KB. Authorization Form for ClinicGroup Billing pdf Use for notification that a practitioner is joining a. The authorization submission process is streamlined by the type of authorization request.
Providers receive a reference number for each prior-authorization submitted. Box 7408 Boise ID 83707-1408 Form No. Complete your Medicare Advantage Prior Authorization Request Form Page 1 above.
Looking for the fastest way to check patient benefits submit a claim or an electronic prior authorization. DATE OF REQUEST Fax. Find change forms for every scenario.
How can we help. Choose how you want to receive or enter your security code. 10-16-1125 the state of Colorado requires carriers and organizations to publish prior authorization data.
Please contact your Provider Relations representative if you have any questions. Provider Prior Authorization Form. Contact your network development representative at the ArkansasBlue welcome center nearest you for assistance.
You can give someone you trust the right to act on your behalf. Contact Bright HealthCare Provider Services.