This tool does not reflect benefits coverage nor does it include an exhaustive listing of all noncovered services in other words experimental procedures cosmetic surgery etc refer to your provider manual for coveragelimitations. Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient medical or behavioral health.
Https Mss Anthem Com California Mmp Caca Mmp 2020coveragedeterminationform Eng Pdf
Prior authorization requirements will be added for the following codes.
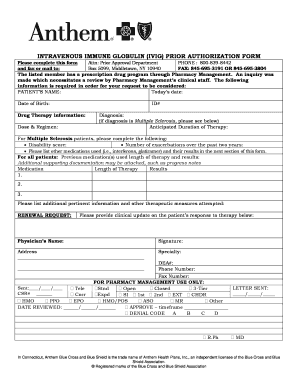
Anthem bcbs prior authorization list. Trades as Anthem Blue Cross and Blue Shield in Virginia and its service area is all of Virginia except for the City of Fairfax the Town of Vienna and the area east of State Route 123. These lists are not exhaustive. Inpatient services and nonparticipating providers always require prior authorization.
E0731 Conductive garment for Tens. Anthem Blue Cross and Blue Shield Serving Hoosier Healthwise Healthy Indiana Plan and Hoosier Care Connect Reminders and updates The provider manual is designed for network physicians hospitals and ancillary providers. Georgia Local PrecertificationPrior Authorization List Updated.
E0730 Transcutaneous electrical nerve stimulation TENS device four or more leads. C1764 Event recorder cardiac implantable E0720 Transcutaneous electrical nerve stimulation TENS device two lead localized. The Precertification Lookup Tool will let.
Our goal is to create a useful reference guide for you and your office staff. We want to help you navigate our. Blue Cross Blue Shield of.
You can access the Precertification Lookup Tool through the Availity Portal. Services Requiring Prior Authorization The table below outlines the services that require Prior Authorization PA for Anthem Blue Cross Medicaid Business members enrolled in Medi-Cal Managed Care Healthy Families Program HMO and EPO Access for Infants and Mothers AIM Program HMO and EPO and Major Risk Medical Insurance Program MRMIP. The procedures or services on the lists below may require prior authorization or prenotification by BCBSTX Medical Management or other designated vendor for certain designated groups.
Anthem Blue Cross and Blue Shield Healthcare Solutions Anthem has an online tool that displays prior authorization guidelines to help you quickly determine whether certain services for Anthem members require a prior authorization. WProsthetic Implant Anthem SURG00023 19328 Removal Intact Mammary Implant Anthem SURG00023 19330 Removal Mammary Implant Matl Anthem SURG00023 19340 Immediate Insertion Breast Prosthesis Following Mastopexy MastectomyIn. Prior Authorizations Lists for Designated Groups.
Request prior authorization review by calling the Blue Cross and Blue Shield Federal Employee Program Service Benefit Plan at 800 860-2156. Anthem expands specialty pharmacy prior authorization list. 010120 19325 Mammaplasty Augmentation.
Anthem Health Plans of Virginia Inc. The Prior authorization list is a list of designated medical and surgical services and select prescription Drugs that require prior authorization under the medical benefit. Anthem Blue Cross and Blue Shield Indiana Medicaid Prior Authorization Requirements Page 2 of 2 Detailed vendor information The Precertification Lookup Tool can be used to look up specific codes for additional detailed vendor information.
Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests. The following guidelines apply to Anthem Blue Cross and Blue Shield Anthem products issued and delivered by Anthem in Connecticut. Anthem FEP will begin accepting prior authorization requests for these specialty drugs on December 14 2020 for dates of service on and after January 1 2021.
Outpatient hospital-based settings will require a site-of. The list below includes specific equipment services drugs and procedures requiring review andor supplemental documentation prior to payment authorization. For information on precertificationprior authorization requirements for those members of National Accounts please call the.
The presence of codes on these lists does not necessarily indicate coverage under. Abraxane Paclitaxel Yes J9264 Preauthorized by Anthem Pharmacy for non-oncology diagnoses and by AIM for oncology diagnoses Actemra Tocilizumab Yes J3262 Preauthorized by Anthem Pharmacy for non-oncology diagnoses and by AIM for oncology diagnoses.