The National Committee for Quality Assurance. Initial Prior Authorization POLICY FDA-APPROVED INDICATIONS Saxenda is indicated as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight.
Https Www Nhpri Org Wp Content Uploads 2020 03 Medicaid Weight Loss Contrave Qsymia Saxenda Criteria20201116 Pdf
O Patients who are actively pregnant or breastfeeding.
Saxenda prior authorization criteria. Prior authorization for prescription drugs is required when your insurance company asks your physician to get specific medications approved by the insurance company. Must meet all of the following. Indicated as an adjunct to a reduced calorie diet and increased physical activity for chronic weight management in adults.
HIV positive patients who have failed traditional antiretroviral therapy defined as those patients who have failed at least 2 susceptible antiretrovirals and whose viral load is more than 5000. Liraglutide Saxenda Lorcaserin Belviq Belviq XR NaltrexoneBupropion Contrave ER Orlistat Xenical Alli Phentermine products PhentermineTopiramate extended-release Qsymia CRITERIA FOR INITIAL APPROVAL. NABP Accredited Digital Pharmacy.
Prior authorization must be provided before the insurance company will provide full or any coverage for those medications. CVS Caremark Criteria Type. The branded products Saxenda BelviqBelviq XR Contrave Xenical and Lomaira are all non formulary.
Drug Name select from list of drugs shown Qsymia phentermine-topiramate Quantity Frequency Strength. The Summary of UM Program Changes captures UM recommendations for any new products molecular entities formulations generics as well as updates to any existing UM programs. MANUAL GUIDELINES The following drugs require prior authorization.
Please click on the link below to search for individual criteria for use. When conditions are met we will authorize the coverage of Anti-Obesity Agents FA-PA. INITIAL COVERAGE If approved initial coverage will be for 18 weeks Liraglutide Saxenda may be eligible for coverage when the following criteria are met.
The medicine can only be obtained with a prescription. Members 18 years of age or older AND As an adjunct to a. The patient has been receiving the requested drug for at least 16 weeks AND The patient lost at least 4 percent of baseline body weight OR the patient has continued to maintain their.
Please find the forms available in alphabetical order of. It is given as an injection under the skin in the thigh upper arm. Please contact CVSCaremark at 1-855-240-0536 with questions regarding the prior authorization process.
Clinical Guidance - Criteria For Use The content on this page has been incorporated into the VA National Formulary Search Tool. URAC Accredited Pharmacy Benefit Management Expires 11012022. The requested drug will be covered with prior authorization when the following criteria are met.
This document is published once a month after every PT meeting. URAC Accredited Mail Service Pharmacy Expires 11012023. Prior Authorization Process and Criteria.
The Georgia Department of Community Health establishes the guidelines for drugs requiring a Prior Authorization PA in the Georgia Medicaid Fee-for-ServicePeachCare for Kids Outpatient Pharmacy Program. Saxenda and Victoza both contain the same active ingredient liraglutide and therefore should. Prior authorization criteria Additionally must be unable to take buprenorphinenaloxone as indicated by ONE of the following.
Requests for special authorization are considered for clients who meet the following criteria. Used in conjunction with a formulary the Prior Authorization Program allows plan sponsors to limit the use of certain drugs by requiring patients to obtain a prior authorization before coverage is issued. The patient has a body mass index BMI 30 kgm2.
Saxenda is injected once per day preferably at the same time every day. 13 years and older b. Indication for Prior Authorization.
No weight loss agent was selected for addition to the Basic Core F ormulary BCF. Saxenda is available as a solution for injection in pre-filled pens. Homozygous familial hypercholesterolemia HoFH AND ALL of the following.
Provided documentation medical records patients chart of confirmed. Designated as Uniform Formulary. What Does Prior Authorization Mean.
Repatha FEP Clinical Criteria Pre - PA Allowance None _____ Prior-Approval Requirements Diagnoses Patient must have ONE of the following. SAXENDA liraglutide injection Status. Saxenda is not indicated for the treatment of type 2 diabetes mellitus.
Saxenda liraglutide PA Required Initiation of Contrave naltrexone HCl and bupropion HCl or Saxenda liraglutide may be approved for up to 12 weeks when all of the following criteria are met. Patient is 18 years of age or older. All the weight loss agents require manual prior authorization patients must try behavioral modification first.
Https Professionals Optumrx Com Content Dam Optum3 Professional Optumrx Resources Pdfs Orxcommforms Anorexiants Comm Pdf
Https Www Medmutual Com Media Medmutual Files Providers Prior Auth Rx Saxenda Pdf
 Nda Saxenda Liraglutide Rdna Origin Injection Novo Nordisk Inc 800 Scudders Mill Road Plainsboro Nj Phone Pdf Free Download
Nda Saxenda Liraglutide Rdna Origin Injection Novo Nordisk Inc 800 Scudders Mill Road Plainsboro Nj Phone Pdf Free Download
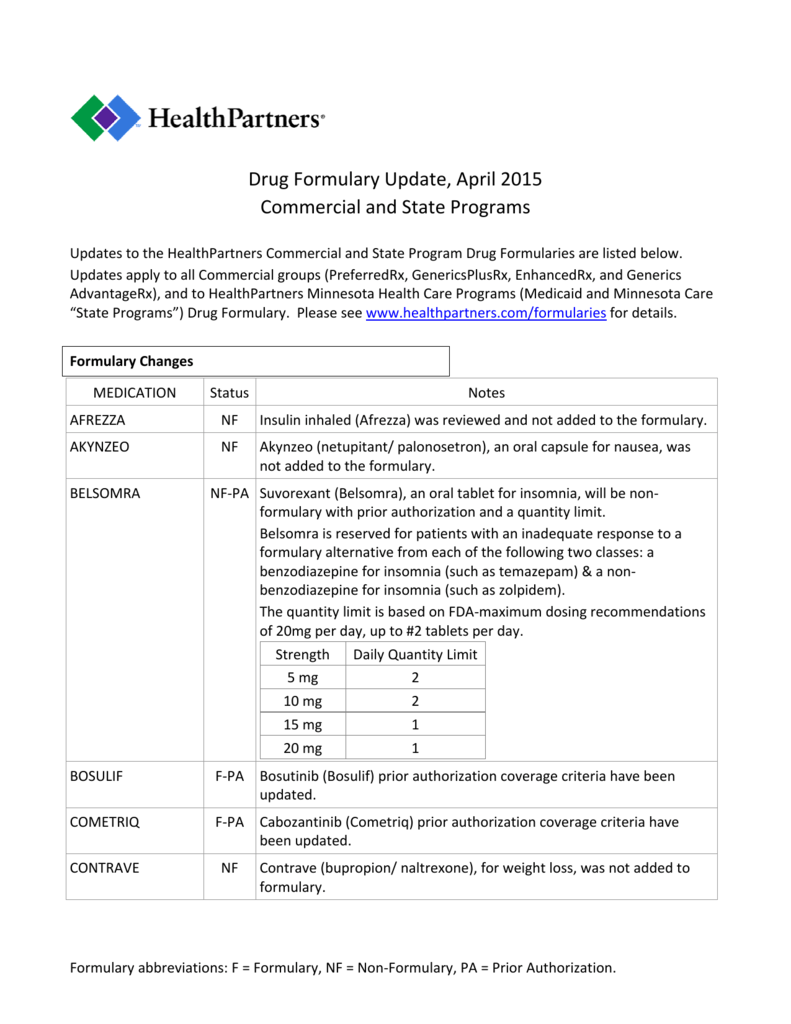 Drug Formulary Update April 2015 Commercial And State Programs
Drug Formulary Update April 2015 Commercial And State Programs
Https Www Nhpri Org Wp Content Uploads 2019 04 Weight Loss Medication Criteria Pa 1 Pdf
 Fillable Online Prior Authorization Program Form Saxenda Nexgenrx Fax Email Print Pdffiller
Fillable Online Prior Authorization Program Form Saxenda Nexgenrx Fax Email Print Pdffiller
Https Www Bluecrossma Com Common En Us Medical Policies 572 20drugs 20for 20weight 20loss 20prn Pdf
Https Www Bluecrossmn Com Sites Default Files Dam 2018 12 P11ga 13885364 2 Pdf
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E174384 Pdf Na Pharminfo
Https Www Healthnet Com Content Dam Centene Healthnet Pdfs Provider Ca Policies 1425 Pdf
Https Martinspoint Org Media Providers Documents Tricare Prior Authorization Forms Saxenda Prior Authorization Form Ashx
 Nda Saxenda Liraglutide Rdna Origin Injection Novo Nordisk Inc 800 Scudders Mill Road Plainsboro Nj Phone Pdf Free Download
Nda Saxenda Liraglutide Rdna Origin Injection Novo Nordisk Inc 800 Scudders Mill Road Plainsboro Nj Phone Pdf Free Download



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.