Thats why we offer a discounted rate on Petplan insurance. Dont get in a fight with them about homebirth.
 Blue Cross Blue Shield Pet Insurance Review Petinsuranceu
Blue Cross Blue Shield Pet Insurance Review Petinsuranceu
BONE CANCER PET scanning may be considered medically necessary in the staging or restaging of Ewing sarcoma and osteosarcoma.

Does blue cross blue shield cover pets. Learn about pet plan Its Your Identity Protect It. So lesson number one. With Petplan pet insurance you wont have to worry about being able to afford care.
Blue Cross- Blue Shield members get a 10 discount when enrolling in Petplan. From what I have read on this site BCBS goes along with Medicare which doesnt cover PETS. No Blue CrossBlue Shield coverage for NDs.
In almost all cases if you call your insurance company and ask if the cover homebirth they will say absolutely not. While BCBS plans can vary based on which state you are in most plans are broken into 3 levels. It is a federation of 36 unique health insurance companies that provide services over the 50 states and over 170 countries.
Blue Cross Blue Shield is known for providing exceptional healthcare insurance throughout the United States. It is typically not possible to obtain insurance coverage for a tummy tuck even if you have diastasis recti. However a higher copay is typically involved with such visits and not all services are covered.
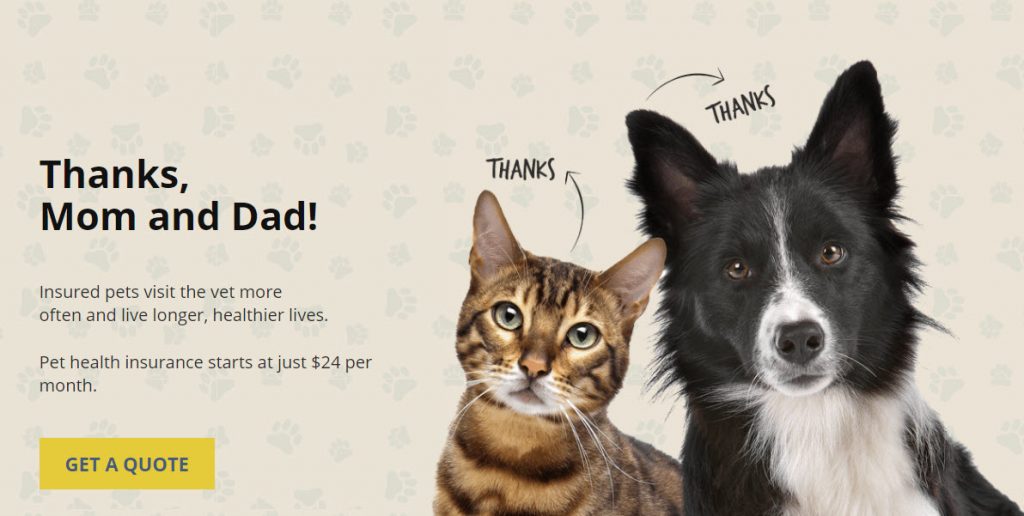
This is why its important to examine your individual plan to find out for certain. When you purchase pet insurance you receive a 10 discount which covers costs associated with routine veterinarian visits treatment for illness or chronic conditions and emergency care plus testing vaccines medications and more. In this way PPO plans offer more flexibility than do HMO plans.
Now I am beginnning to deal with Medicaid and that is a new challenge as my COBRA Blue CrossShield expires 812010. FINALLY I can say that I appear not to have had any PET scans so Blue CrossShield didnt need to pay. Hope you are doing well.
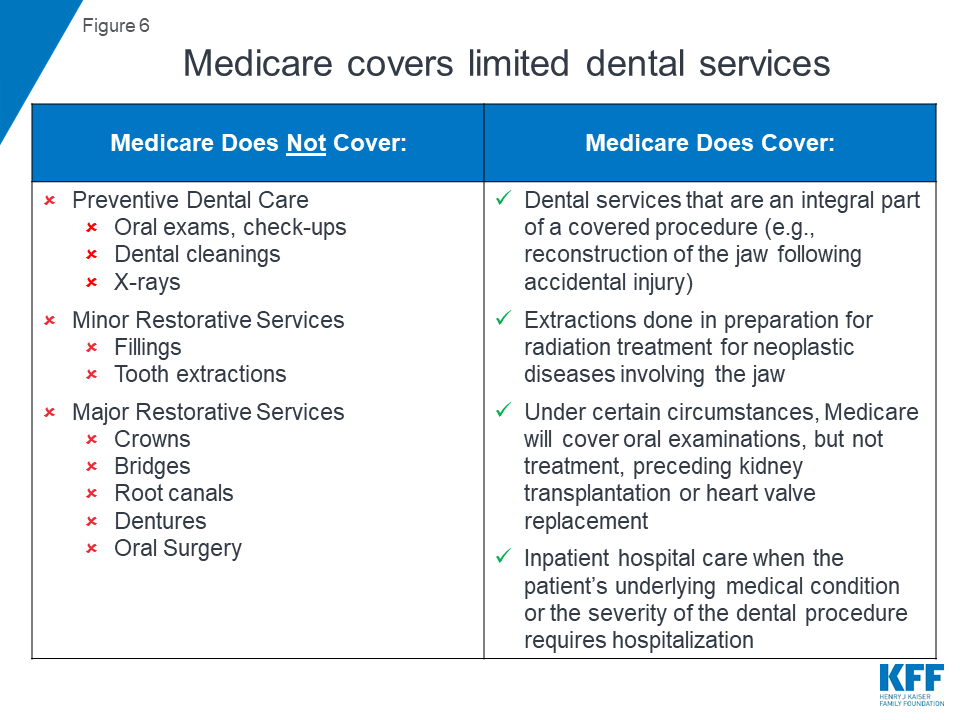
Your dental benefit plan does not cover services supplies drugs or charges that are. At the most basic level insurance companies are denying PET scans because they cost up to 8x as much as CT scans and about 2-4x as much as MRI scans--However there are reasons aside from cost for having one type of scan vs another---I had the opportunity last spring to sit for over an hour with an excellent radiologist who reviewed all of my scans with me a total body PET about 3200. Depending on the plan you have Blue Cross Blue Shield may cover up to one hundred percent of your stay at an inpatient drug and alcohol treatment center.
I appear to have had CT MRI MRCP and Ultrasound. Most other companies will reimburse patients at an out-of-network rate. I have asked for info from BS but until that arrives does anyone know anything.
At Blue Cross Blue Shield of Massachusetts we want our members and their pets to be healthy. BCBS is an association that has been providing healthcare since 1982. Bronze plans have the lowest premiums but out-of-pocket costs are higher.
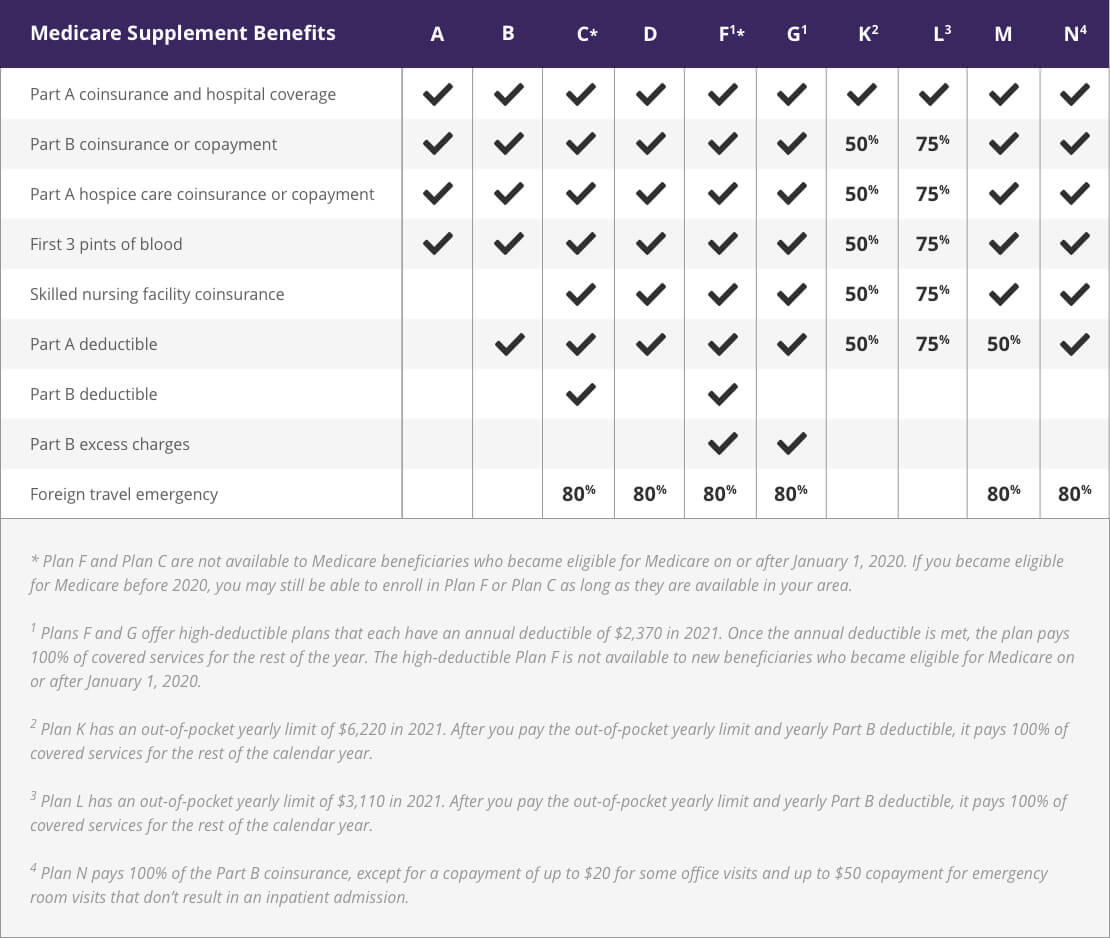
Blue Cross Blue Shield requires adherence and will only cover a medically necessary PAP device beyond the first three months of therapy when PAP use is greater than or equal to 4 hours per night on 70 of nights during a consecutive 30 day period during the first three months of therapy. Does anyone know if Blue Shield covers PETS in CA. BCBS pays about 60 of the costs of your medical care once your deductible is met.
95 of the doctors and hospitals in the USA recognize and associate with Blue Cross Blue Shield. The other option is just head over to the Petplan. The discount is only offered on the Blue Cross Blue Shield website.
There are more Anthem blue cross. Their coverage comes through Petplan their insurance partner. Get Help Now 100 confidential free.
Supply is medically necessary does not constitute a representation or warranty that the Blue Cross and Blue Shield Service Benefit Plan covers or pays for this service or supply for a particular member. Leila Kasrai MD FRCSC Certified Plastic Surgeon. 2 days ago Nov 17 2020 If you are already a Blue Cross Blue Shield plan member you can add Petplans insurance to your own health pet insurance to have all your family including pets coverage in one place.
A tummy tuck is considered a cosmetic procedure. Blue Cross Blue Shield members who are covered under a PPO plan may visit any health care professional physician or specialist they choose without a referral from their primary care doctor. I am needing to consider changing insurance companies due to geography issues.
About Blue Cross Blue shield. As of November 24 2020 Health Care Service Corporation the second-largest Blue Cross Blue Shield licensee operating in Illinois Texas Montana New Mexico and Oklahoma announced a new lipedema coverage policy. Just let your midwife bill usually she does not indicate the location of the birth and it will get covered.
Blue Cross Blue Shield Pet Insurance Review PetInsuranceU. Not all pet insurance is the same so its important to check the cover provided for veterinary care carefully and choose the right provider for you and your pet. Copays and deductibles vary greatly between plans and levels.
PPO plan members may also see doctors outside of their network. Not only does each separate BCBSA company differ in their coverage but they also offer a variety of different levels of care each with varying hearing health coverage. Your costs can be covered.
All Patients must check their specific insurance health plan if a specific naturopathic doctor andor Group is listed otherwise an ND andor Group. Your Furry Friend Deserves Care Protection Too. Blue Shield is my option but I currently get PETs several times a year with Kaiser as my CA -125 is not a marker I can use.
While this policy has many requirements for coverage we believe that our Coverage Process is well suited to. And did you know that Blue Cross Blue Shield also offers pet insurance. All dogs cats and rabbits rehomed from Blue Cross come with four weeks free Petplan insurance.
It offers coverage for most medical procedures. Blue Cross Blue Shield Rehab Coverage Levels and Plans.