PPO plans include out-of-network benefits. We provide health insurance in Michigan.
 Blue Connect Blue Cross And Blue Shield Of North Carolina
Blue Connect Blue Cross And Blue Shield Of North Carolina
Cases in which Blue Shield of California Medicare health plan authorizes use of out-of-network providers You are responsible for paying the full cost of services of unauthorized out-of-network services.
Blue cross blue shield out of network coverage. As a member of an employer plan you can find doctors in our network across the US. You present your ID card to the provider who submits your claim to the local Blue plan. For example your plan may pay 80 percent and you pay 20 percent if you go to an in-network doctor.
They help pay for care you get from providers who dont take your plan. In the United States Puerto Rico and US. If no one in the network can give you the care you need your primary care provider PCP will get an OK from us to send you to a provider that is not in the network.
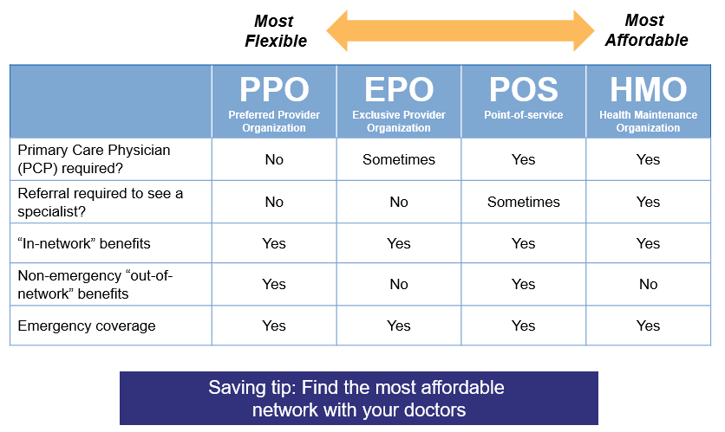
If you have an HMO plan you are only covered for in-network care except in medical emergencies when you may receive coverage out-of-network. In most cases you must receive your care from a CHIP in-network plan provider. The first feature that youll want to check out is the security manager which helps you manage your user access privileges.
You may pay more or for all of your health care costs if your provider is out of your network or does not have a contract with Blue Cross this is called a nonparticipating provider. By choosing Student Blue SM you get. Access to a large provider network with coverage in all 100 counties in North.
In fact the BlueCard network includes 95 of care providers in the United States. Search for Doctors Hospitals and Dentists Blue Cross Blue Shield members can search for doctors hospitals and dentists. When you receive health care from a PPO network provider you enjoy maximum coverage and convenience.
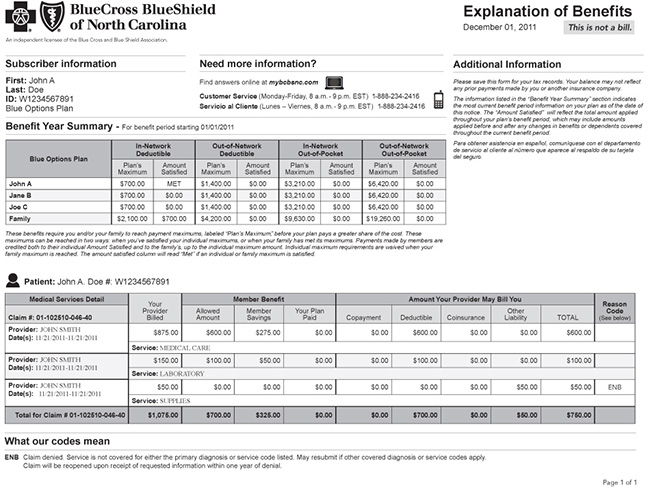
A member can notify Arkansas Blue Cross prior to receiving a health intervention from a non-preferred provider and if Arkansas Blue Cross determines that the required covered services or supplies associated with the health intervention are not available from a preferred provider and provide a written approval of in-network coverage for such services or supplies in-network deductibles coinsurance and copays will apply to the claims for the services. You can verify if your provider is in your network by calling customer service at the number on the back of your member ID card. You may have to pay the out-of-network provider in full and submit your own claim to Blue Cross NC.
A health plan from the most trusted health insurer in North Carolina 1. The most important thing is that whatever BCBS does. Out-of-Network Care is care you receive from.
The coverage your plan offers for in-network and out-of-network health care providers and the network your provider is in both impact how much you pay for care. The local plan works with Highmark Blue Cross Blue Shield to ensure prompt and accurate claims payment. Our Point-of-Service POS will cover services from out-of-network providers as long as the services are covered benefits and are medically necessary.
Out of network your plan may 60 percent and you pay 40 percent. Its the widely accepted coverage and superior service from fellow North Dakotans at 10 offices across the state. Find Coverage The my Blue Group Agent Member Pharmacy and Provider portals will be unavailable Saturday May 15th from 600 PM until 900 PM.
Now that your permissions are in place use our employee maintenance tools to tackle that to do list even more quickly. Student Blue SM from Blue Cross and Blue Shield of North Carolina BCBSNC provides quality health insurance to meet the specific needs of university students. Use the security manager to add and delete authorized users assign security permissions and reset passwords as needed.
This company is committed to high quality medical care and this also includes mental health and substance abuse coverage. If you have BCBS insurance finding a rehab center shouldnt be too difficult. Why are Blue Cross Blue Shield of North Dakota members among the most satisfied in the nation.
Blue Cross is part of the national BlueCard network. 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States.
For emergency or urgent care you do not need to get an OK from us. Please refer to Chapter 3 of your plans Evidence of Coverage for full information on out-of-network medical coverage. If no one in the network can give you the care you need your primary care provider PCP will get an OK from us to send you to a provider that is not in the network.
In most cases you must receive your care from a STAR in-network plan provider. Claims not received within 18 months from the service date will not be covered except in the absence of legal capacity of the member. Blue Cross Blue Shield has been providing millions of people with insurance coverage for over 80 years.
The Blue Cross Blue Shield Global Core network for employer plans offers access to. National and international coverage for employer plans. Please plan to visit these sites either before or after that time.
But you usually pay more of the cost. Outside the United States. This benefit has a coverage maximum of 3000 each calendar year.
Claims must be received by Blue Cross NC within 18 months of the date the service was provided.








.jpg)

