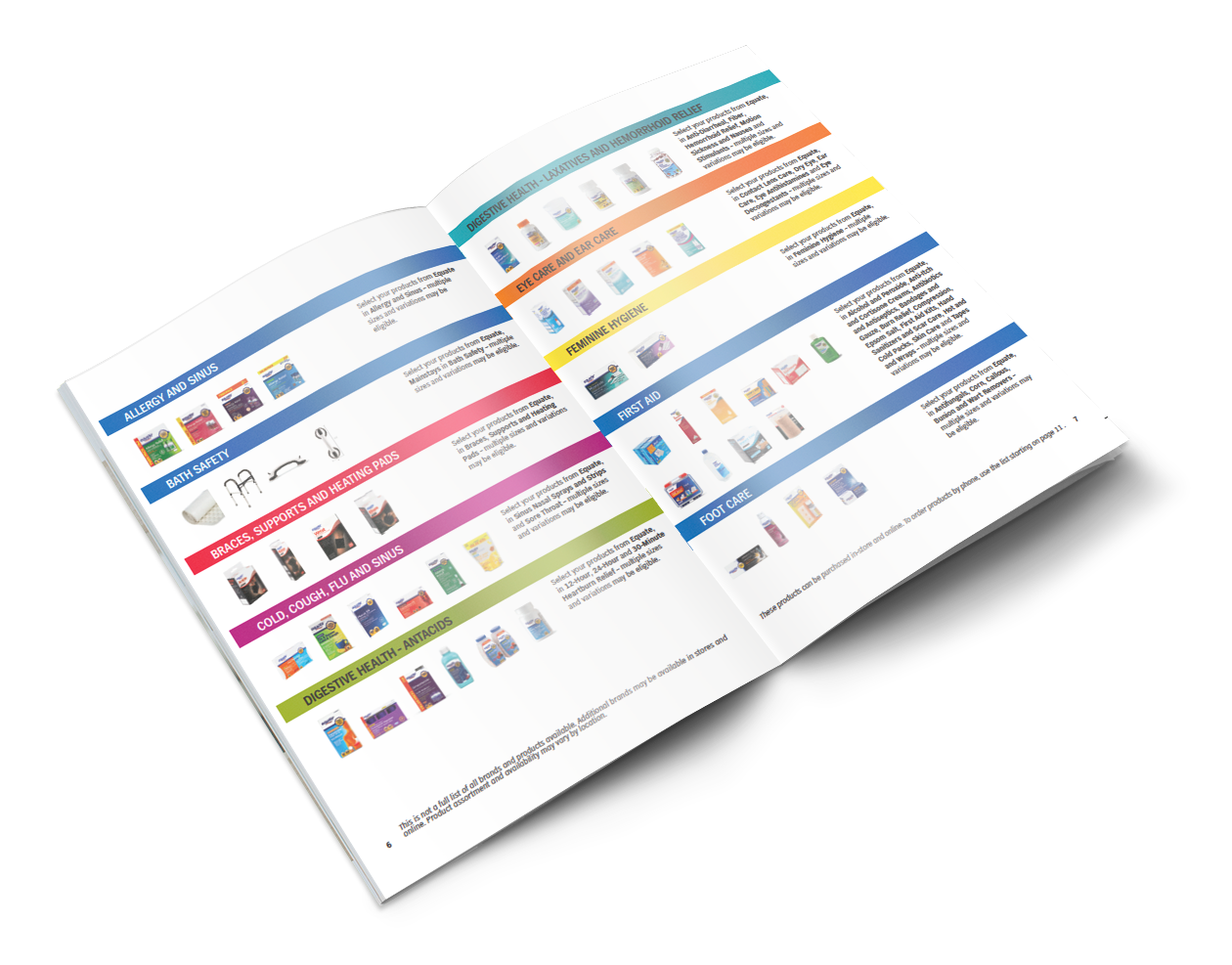
Benefit Overview It can be used to purchase over-the-counter OTC eligible items that help treat injuries or illness. You can use your OTC card for covered items at participating local retailers and stores.
 2021 Benefits Card Otc Program
2021 Benefits Card Otc Program
You can use your card to buy most health products as well as medications.
Otc card eligibility. These cards can be used to purchase most OTC products and medications. As a member of ArchCare Advantage HMO Special Needs Plan you will get a pre-paid Over-the-Counter OTC card. Enter your 19-digit OTC.
The online portal allows patients to perform the following tasks. Yes discounts are available regardless of item eligibility. For added convenience download the OTC Network app to scan products in stores to determine eligibility and check your card balance.
You can use your OTC Card to buy over-the-counter OTC and heath-related items. In 2021 the OTC card benefit is 120 per month up to 1440 per year. The CARES Act of March 2020 expanded the benefits of HSAs and FSAs by removing the prescription requirement for several OTC drugs and medicines and by adding feminine hygiene products to the list of expenses eligible for reimbursement.
ICare Medicare Plan HMO D-SNP members will receive 100 per month 1200 per calendar year to purchase OTC items approved non-prescription drugs and health-related items. For a complete list of eligible items please see 2021 OTC and Grocery Program Catalog or call us. It can be used to purchase over-the-counter OTC eligible items that help treat injuries or illness.
PLAN BENEFIT BlueCHiP for Medicare Advance HMO 25 quarter BlueCHiP for Medicare Core. Here are some common questions members ask about the OTC and Grocery Program benefit. Batteries hearing aid Cold Allergy.
Your insurance carrier is in charge of reloading your card each month. Plus you may be eligible for additional benefits on either Assistive Devices or Service Dog Support items. You can use this card to buy eligible over-the-counter OTC medicines and health-related items.
Your Over-the-Counter OTC and Grocery Card. Shaving cream and razors. As a member of VNSNY CHOICE Total HMO D-SNP you are covered for up to 132 a month for OTC and Grocery items.
You can use this card to purchase many common items at local pharmacies including CVS Walgreens Rite Aid and Duane Reade without having to submit a receipt. Oral teething pain treatment. Please note that an expense is only considered eligible for FSA reimbursement if it is deemed medically necessary to treat a specific medical condition disease or diagnosis.
Any remaining balance at the end of the month will not carry over to the next month. Stomach upset medicinedigestive aids. For more information view your Evidence of Coverage or contact Member Services.
Any unused balance will automatically expire at the end of each quarter or upon disenrollment from the plan. Check on the card balance. Call 1-888-682-2400 TTY 711 to check your balance.
View all the participating retailers available. You can use this card. OTC over-the-counter items are available without a prescription or simply over the counter OTC drugs are in contrast to prescription drugs that require a doctors order.
To get started activate your card. Here are 10 things you didnt know you could buy with your OTC card. Most major retail stores accept these cards so you shouldnt face difficulty in using it.
Eligible items up to your available balance amount will be covered. Use your debit card at all Walmart Dollar General Family Dollar Rite Aid Walgreens and CVS Pharmacy retail stores. Once you exceed your allowance average of 50-100month for most providers the card is no longer valid until it is reloaded by your insurance provider.
Welcome to your OTC Network cardholder portal. Whether you buy through a store or your catalog a wide variety of products are OTC-eligible in categories including. Eligible OTC Card Members have access to a free and secure online card management tool.
Your card will only work for covered items at participating stores. Thanks to Anthem BlueCross BlueShield you receive benefits on a variety of over-the-counter OTC health items you use every day. Certain Medicare Advantage plans offer beneficiaries a unique way to buy over the counter products.
This means you can now use your HSA or FSA to reimburse yourself for several everyday items or if you have a. Can I still get a discount even if the item is not eligible for purchase with my OTC Card. A Medicare Advantage over the counter drug card is a prepaid card for products.
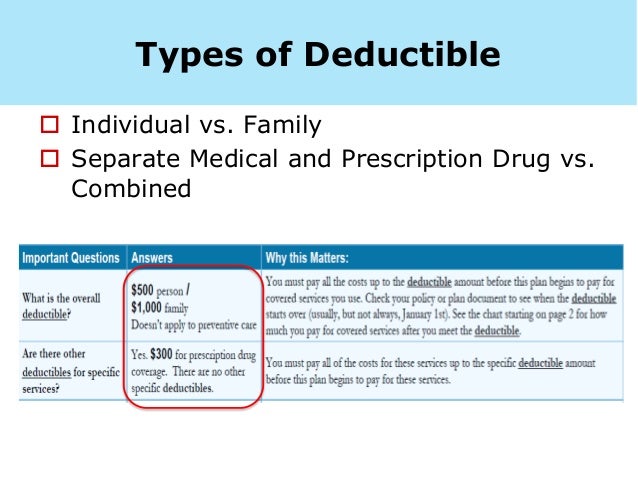
If there is an in-store discount on an eligible savings item will I still receive the OTC Network discount. OTC items may be purchased only for the enrollee. Depending on your plan you will receive an OTC card with a maximum limit for purchasing approved OTC nonprescription drugs health-related items at participating pharmacy locations and in the case of Life Improvement Plan and CompleteCare healthy foods and produce items.
You can use this card to purchase many common items at local pharmacies including CVS Walgreens Rite Aid and Duane Reade without having to submit a receipt.