One of the goals of the program is to promote better access to services for beneficiaries through the integration of behavioral and physical health. For our Cal MediConnect members Community Health Group covers inpatient and outpatient treatment.
 New Resource Demystifies Medi Cal S Mental Health Coverage Under The Aca California Health Care Foundation
New Resource Demystifies Medi Cal S Mental Health Coverage Under The Aca California Health Care Foundation
Are your Medicare mental health services covered.
Mental health services covered by medi cal. The Affordable Care Act ensures that all Medi-Cal health plans offer a comprehensive package of services known as essential health benefits Essential health benefits must include. The following substance use disorder services benefits will also be made available to eligible Medi-Cal beneficiaries. Individual and group mental health evaluation and treatment psychotherapy rendered by a psychologist LCSW or MFT Psychological testing when clinically indicated to evaluate a mental health condition.
Sometimes these services are available through your regular doctor. Early and Periodic Screening Diagnostic and Treatment EPSDT is a Medi-Cal benefit for individuals under the age of 21 who have full-scope Medi-Cal eligibility. Medi-Cal Mental Health Services Referral Processes.
Mental Health Services Recipients who are eligible for Medi-Cal mental health services may receive the following. Voluntary Inpatient Detoxification Intensive Outpatient Treatment Services Residential Treatment Services Outpatient Drug Free Services. Some states like Virginia offer substance use disorder services as part of their Medicaid plans.
These services are for the treatment of mild to moderate mental health conditions which include. Mental Health Services Services such as individual and group mental health evaluation and treatment psychological testing certain outpatient services including laboratory drugs supplies and supplements and psychiatric consultation. Ambulatory patient services 2.
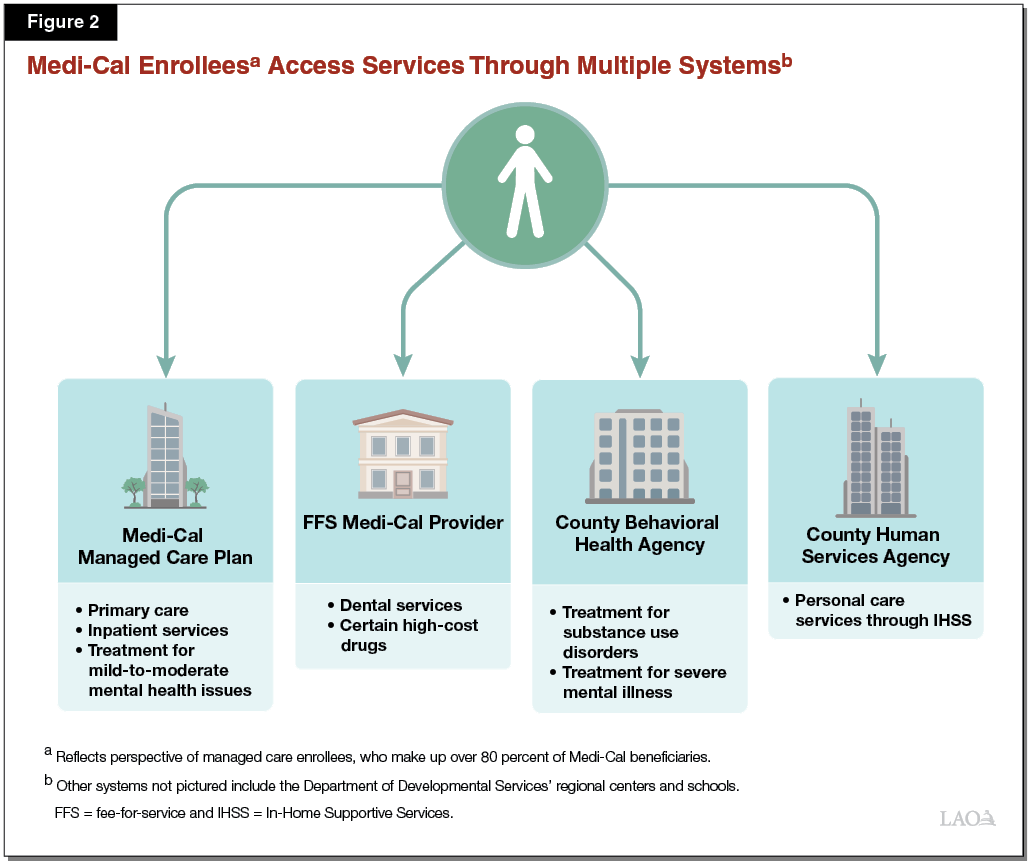
Mental health services are delivered in the Medi-Cal program through a systemor set of local public systemsdistinct from other Medi-Cal services. In Virginia those who use Medicaid FAMIS and FAMIS MOMS are covered for Addiction and Recovery Treatment Services known as ARTS. MHPs have a memorandum of understanding MOU with each MCP that enrolls beneficiaries covered by.
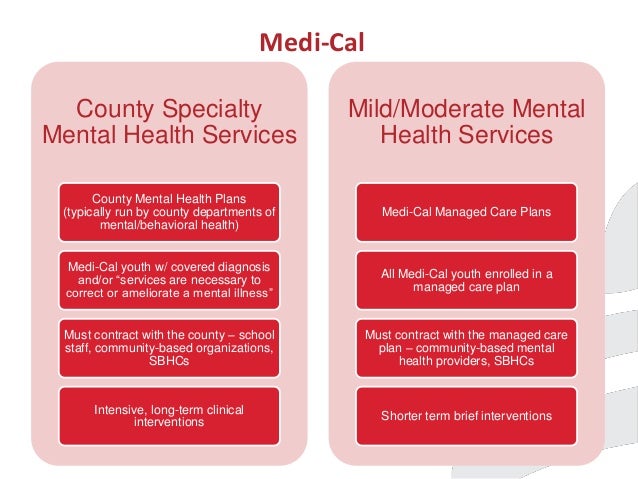
The Medi-Cal Specialty Mental Health Services SMHS program is carved-out of the broader Medi-Cal program and operates under the authority of a waiver approved by the Centers for Medicare and Medicaid Services CMS under Section 1915b of the Social Security Act. TARs for psychiatric inpatient hospital services to the countys Mental Health Plan MHP. Recipients that meet medical criteria for specialty mental health services will receive mental health services via county MHPs.
EPSDT provides periodic screenings to determine health care needs and. This consolidation affects psychiatric inpatient hospital services only. The MHP authorizes psychiatric inpatient hospital service admissions continued stay services and administrative days for all Medi-Cal recipients based on county of residence.
Medi-Cal beneficiaries enrolled in Medi-Cal Managed Care Plans MCPs may receive mental health services via their MCP or specialty mental health services SMHS through their County Mental Health Plan MHP if they meet SMHS medical necessity criteria. Mental health services for our Medi-Cal members with a serious mental health condition are covered by the County Mental Health Plan. Outpatient mental health services are now a covered benefit by Molina.
To find out how to get mental health. Individual and group mental health evaluation and treatment psychotherapy. You can call Molina or ask your PCP for the name of a plan mental health provider.
There are no limits on the number of inpatient days in a facility and no limits on the number of outpatient visits. Addiction treatment services and drug rehab programs generally covered through Medi-Cal include. Services covered by Medi-Cal include outpatient mental health services such as individual or group counseling outpatient specialty mental health services inpatient mental health services outpatient substance use disorder services residential treatment services and voluntary inpatient detoxification.
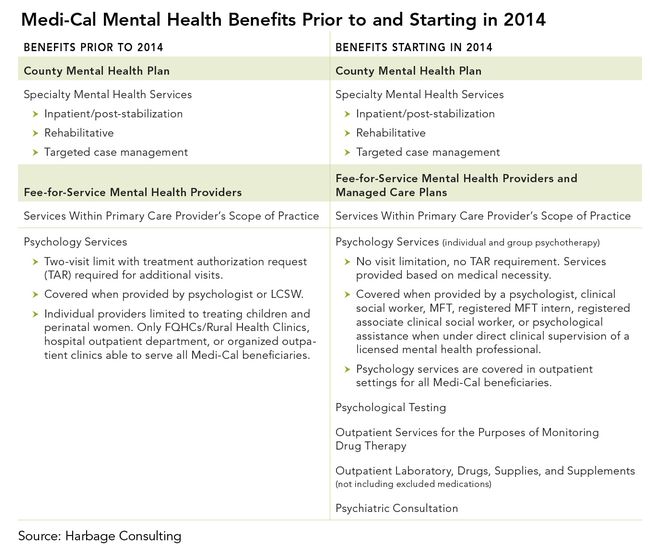
Mental health services have been part of the benefits package for Medi-Cal Californias Medicaid pro-gram since the program was established in 1965. Mental health services are available to people on Medi-Cal including children young people adults and older adults in Contra Costa County. Specialty mental health services currently provided by County Mental Health Plans will continue to be available.
Mental Health and Substance Use Disorder Services including. The Medi-Cal program pays for a significant portion of mental health treatment in California. For seniors with low incomes Medi-Cal also covers services not paid for by Medicare including nursing home care.
MediCal specialty mental health services for children and nonminor dependents who meet medical necessity criteria Transition support services Education and physical behavioral and mental health supports including extracurricular activities and social supports. Most of these mental health and substance use disorder benefits are also available for people in Medi-Cal. Behavior health treatment for children under 21.
Smoking cessation services. Maternity and newborn care. Individual group and family therapy.
As the single state Medicaid agency DHCS is responsible for administering the Medi-Cal SMHS Waiver Program which provides SMHS to Medi-Cal beneficiaries through County Mental Health. Pediatric Services Including Oral and Vision Care. Sometimes they are provided by a specialist and called specialty mental health services.
Mental Health Services Delivery Systems Eligible Medi-Cal recipients may receive Medi-Cal mental health services through all Medi-Cal delivery systems including but not limited to Managed Care and fee-for-service delivery systems.
 Health Insurance And Mental Health Services Mentalhealth Org
Health Insurance And Mental Health Services Mentalhealth Org
 The 2020 21 Budget Re Envisioning Medi Cal The Calaim Proposal
The 2020 21 Budget Re Envisioning Medi Cal The Calaim Proposal
Https Www Chcf Org Wp Content Uploads 2016 08 Circlemedicalmentalhealth Pdf
 The Doctor Is Out Nami National Alliance On Mental Illness
The Doctor Is Out Nami National Alliance On Mental Illness
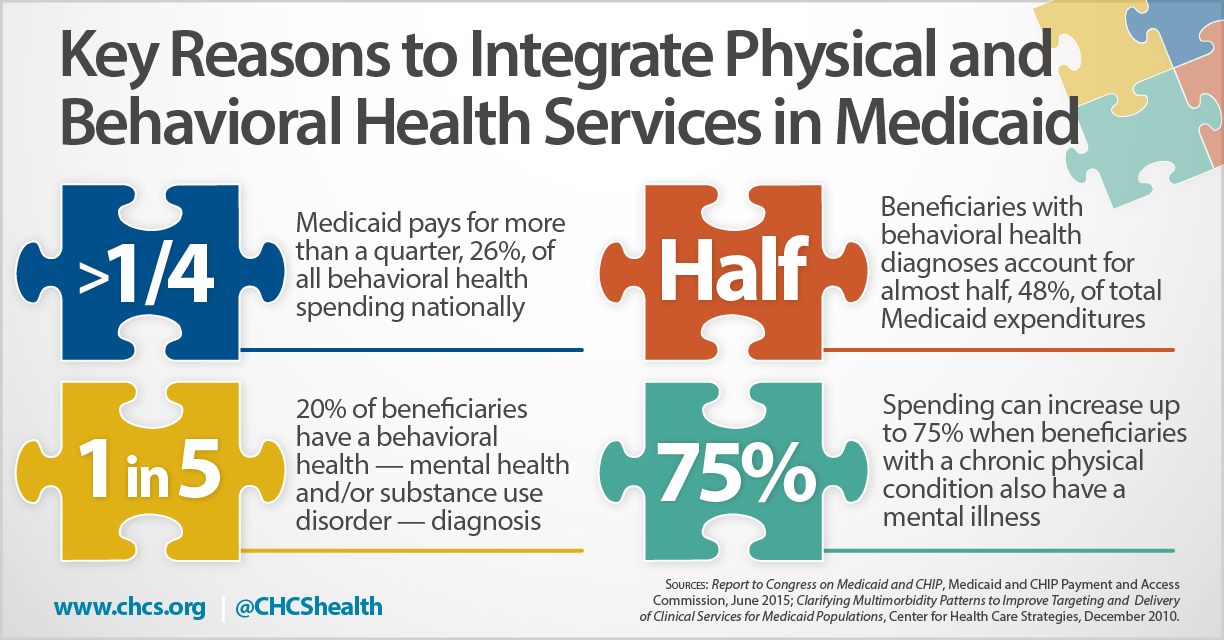 Key Reasons To Integrate Physical And Behavioral Health Services In Medicaid Center For Health Care Strategies
Key Reasons To Integrate Physical And Behavioral Health Services In Medicaid Center For Health Care Strategies
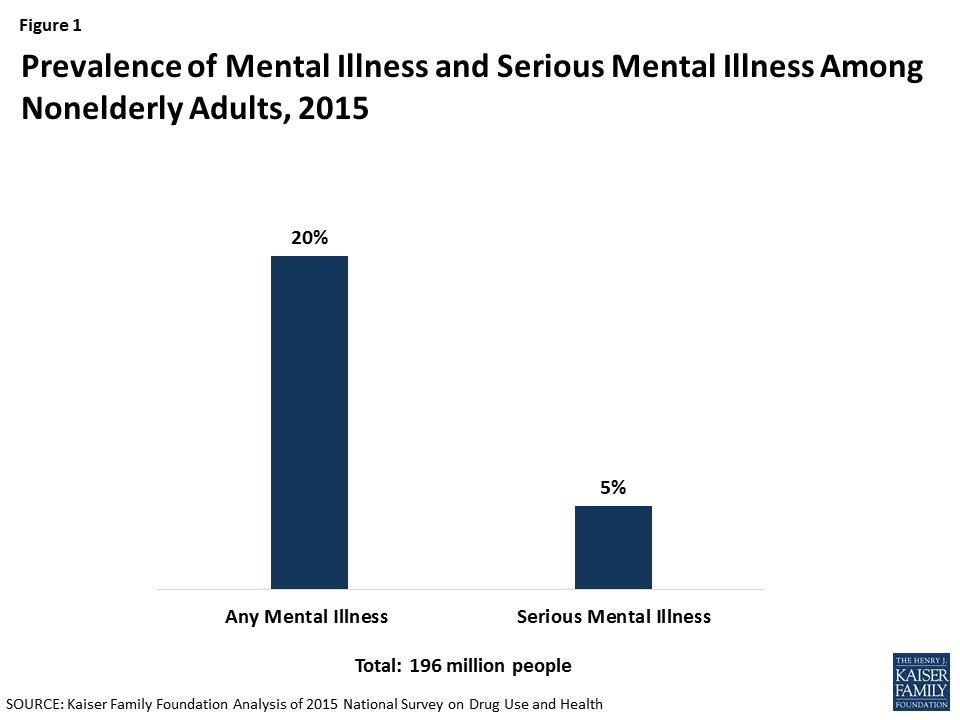
 Facilitating Access To Mental Health Services A Look At Medicaid Private Insurance And The Uninsured Kff
Facilitating Access To Mental Health Services A Look At Medicaid Private Insurance And The Uninsured Kff
Mental Health Parity Nami National Alliance On Mental Illness
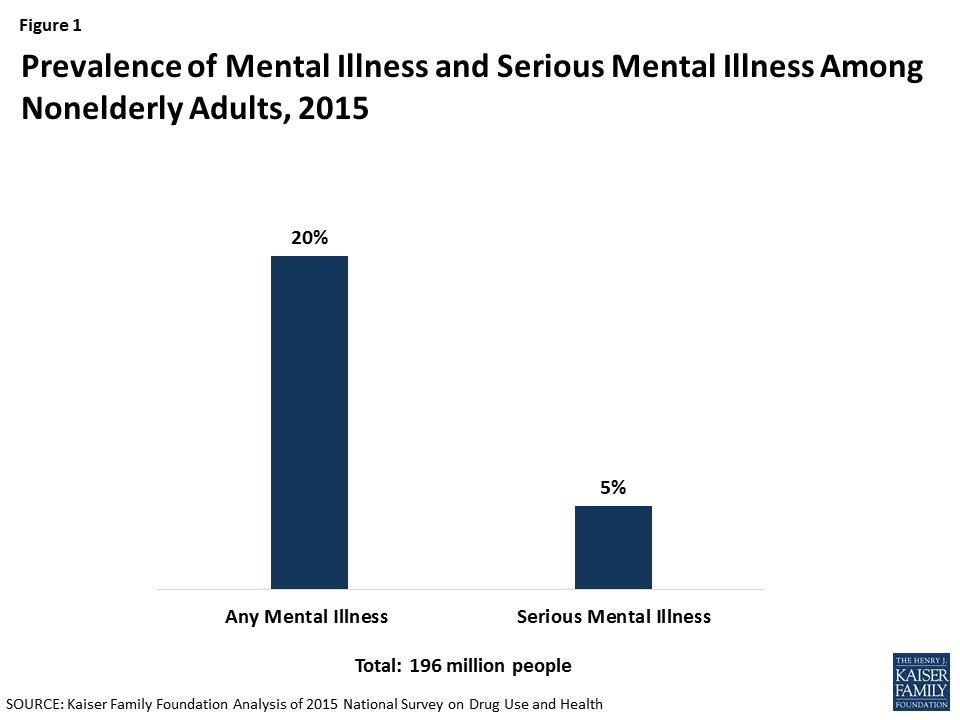
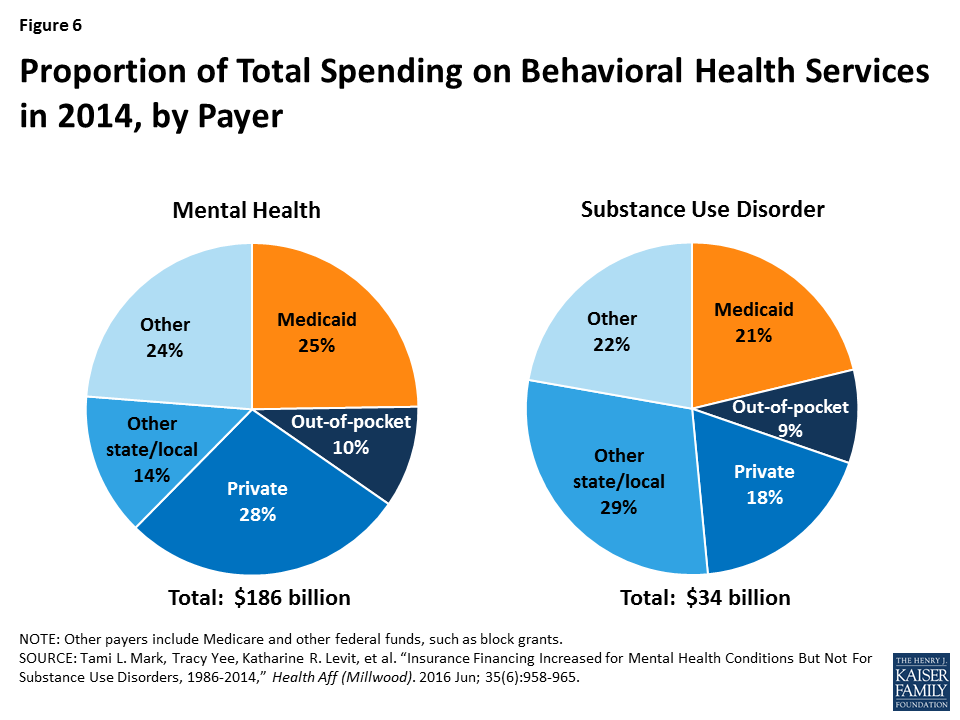 Medicaid S Role In Financing Behavioral Health Services For Low Income Individuals Kff
Medicaid S Role In Financing Behavioral Health Services For Low Income Individuals Kff
 Mental Health Parity Nami Piedmont Tri County
Mental Health Parity Nami Piedmont Tri County
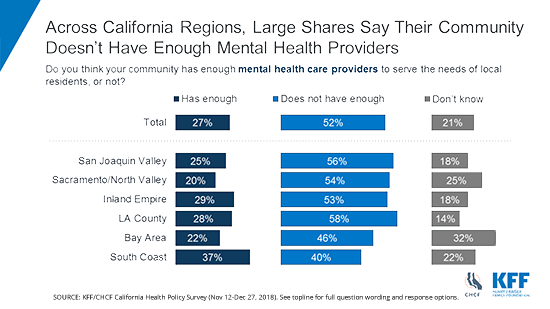 California Poll Access To Mental Health Care Insurance Coverage And Affordability Rank Among Californians Top Health Care Priorities For The New Governor And Legislature Kff
California Poll Access To Mental Health Care Insurance Coverage And Affordability Rank Among Californians Top Health Care Priorities For The New Governor And Legislature Kff
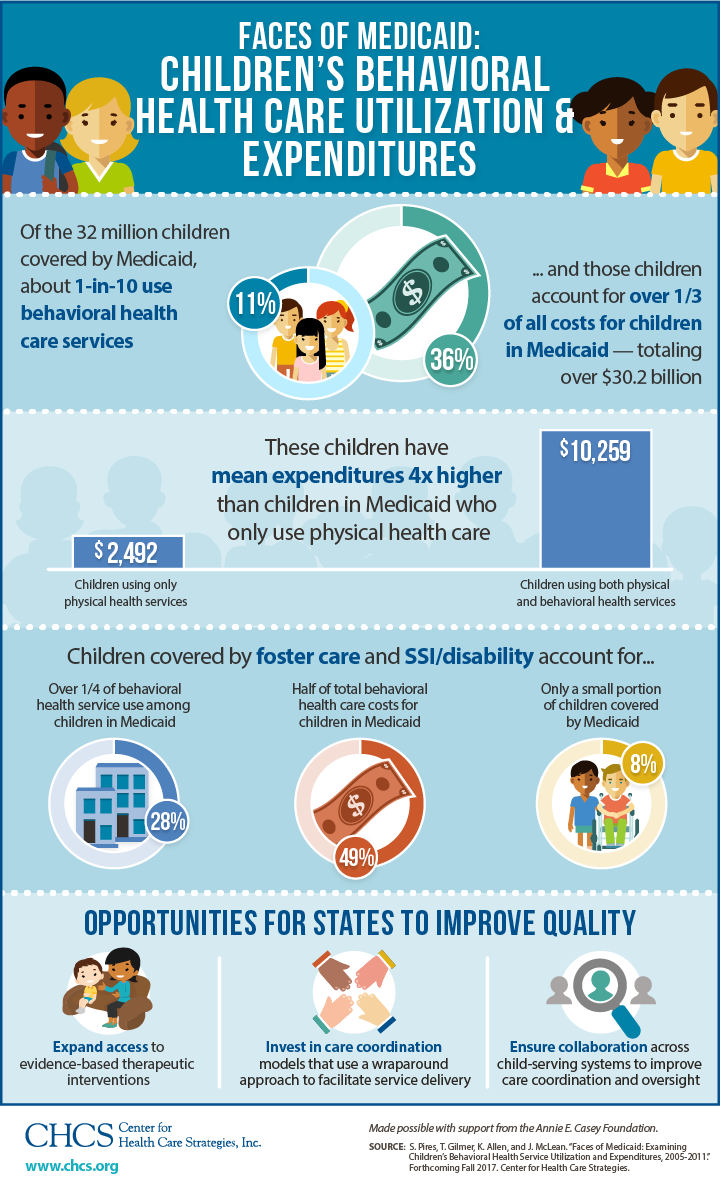 Data Update Children S Behavioral Health Care Use In Medicaid Chcs Blog
Data Update Children S Behavioral Health Care Use In Medicaid Chcs Blog
 Navigating The Challenges Of Medi Cal S Mental Health Services In California An Examination Of Care Coordination Referrals And Dispute Resolution National Health Law Program
Navigating The Challenges Of Medi Cal S Mental Health Services In California An Examination Of Care Coordination Referrals And Dispute Resolution National Health Law Program
 Mental Health Coverage In Us Health Plans Ehealth
Mental Health Coverage In Us Health Plans Ehealth
 Dollars And Cents Public Funding To Sustain School Based Mental Heal
Dollars And Cents Public Funding To Sustain School Based Mental Heal


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.