The Independence Blue Cross network includes both preferred and standard. Food and Drug Administration.
Https Www Ibx Com Documents 35221 56677 Prior Auth Makena Pdf 08bf7ea6 Baa2 Bf95 0587 20c06ca3398f T 1580924446433
HIPAA Personal Representative Request Form appoints another person as members personal representative.
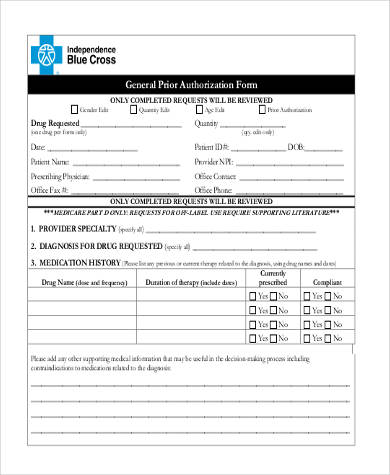
Independence blue cross prior authorization form. Anthem has also made available a series of forms. CRNP and PA direct supervision requirements Billing Reimbursement. Blue Cross Completes prior authorization criteria for a brand-name DAW request.
The Independence Blue Cross pharmacy network allows you to get your prescription filled at over 60000 locations. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Specialist as primary care provider request form.
The approval criteria were developed and endorsed by the Pharmacy and Therapeutics Committee and are based on information from the US. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. A network mail-order pharmacy service.
Submit the completed form. Coordination of Care and Treatment Summary Form. These products will be removed from some formularies and will require a new prior authorization on others effective October 1.
Long-term care and home-infusion pharmacies. A standardized or uniform prior authorization PA form may be required in certain states to submit PA requests to a health plan for review along with the necessary clinical documentation. Reviews from Independence Blue Cross employees about working as a Prior Authorization Specialist at Independence Blue Cross.
Prior Authorization Request Confidential Information June 2020 PH-ANR-25Rev070120. At AIM Specialty Health AIM its our mission to promote appropriate safe and affordable health care. As the leading specialty benefits management partner for todays health care organizations we help improve the quality of care and reduce costs for todays most complex tests and treatments.
They can be printed then completed and signed by hand or they can be filled in on-line printed. Attention Pharmacy at 1-855-811-9326 By mail. For members who have prescription drug coverage through Independence Blue Cross Independence prior authorization is required for certain prescribed formulary drugs in order for such drugs to be covered.
Floor Prior Auth Dept 200 Stevens Drive Philadelphia PA 19113. Learn about Independence Blue Cross culture salaries benefits work-life balance management job security and more. Access the most commonly used forms such as continuity of care requests provider changes HIPAA authorizations and physician referrals.
Basically you may need additional approval from your health plan before you receive certain tests procedures or medications. Request or Refusal for Interpreter Service Form Armenian. Access the most commonly used forms such as continuity of care requests provider changes HIPAA authorizations and physician referrals.
This may also be called preapproval pre-authorization or prior authorization. These standard forms can be used across payers and health benefit managers. Independence drug program formulary updates Pharmacy COVID-19 Coronavirus.
Physician dentist or optometrist who is requesting coverage on your behalf. Independence Blue Cross Independence announced that as part of its commitment to helping reduce opioid misuse and overprescribing it is placing new restrictions on OxyContin and Oxycodone ER. Temporary suspension of certain prior authorizations Medical COVID-19 Coronavirus.
28 Zeilen Prior Authorization Forms Select pharmacy tab Prior Authorization. Request or Refusal for Interpreter Service Form Arabic. In some instances the patient may also be required to sign the forms.
HIPAA Authorization for Disclosure of Health Information authorizes Independence Blue Cross Independence to release members health information. Cultural and Linguistic Referral Form. NoteThese special authorization forms must be completed and signed by an authorized prescriber eg.
Implant Reimbursement Request Form.
 Fillable Online Independence Blue Cross Viscosupplementation Prior Authorization Form Independence Blue Cross Viscosupplementation Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Independence Blue Cross Viscosupplementation Prior Authorization Form Independence Blue Cross Viscosupplementation Prior Authorization Form Fax Email Print Pdffiller
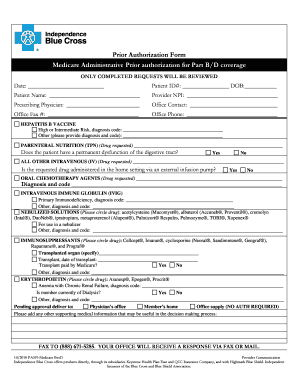
 Independence Administrators Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Independence Administrators Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Https Www Ibx Com Documents 35221 56677 Prior Auth Botulinum Toxins Pdf 99b5b638 Fc7c 290b Ab03 58c7a997ef40 T 1580924446000
 Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
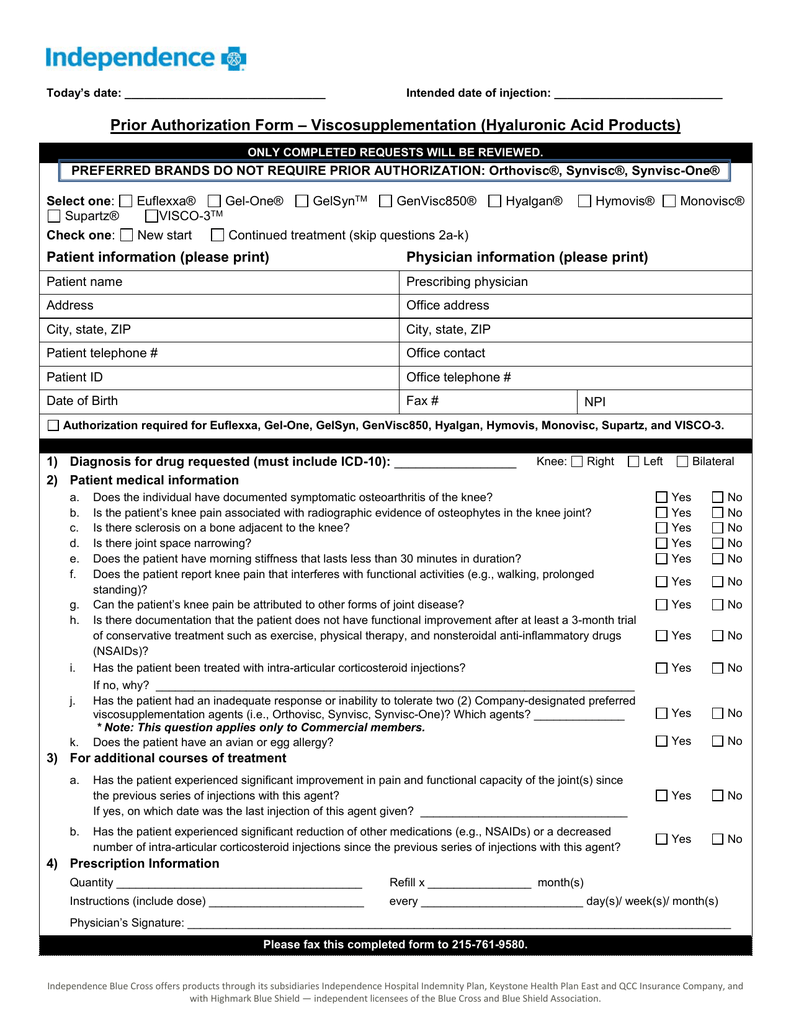 Prior Authorization Form Viscosupplementation Hyaluronic Acid
Prior Authorization Form Viscosupplementation Hyaluronic Acid
 Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
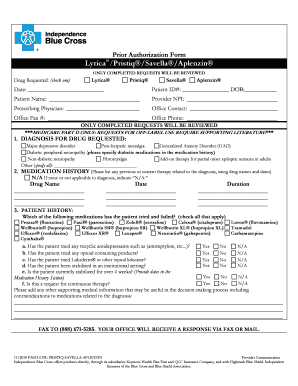
 Bcbs Prior Auth Forms To Print Fill Online Printable Fillable Blank Pdffiller
Bcbs Prior Auth Forms To Print Fill Online Printable Fillable Blank Pdffiller
 Prior Authorization Form Independence Blue Cross Printable Pdf Download
Prior Authorization Form Independence Blue Cross Printable Pdf Download
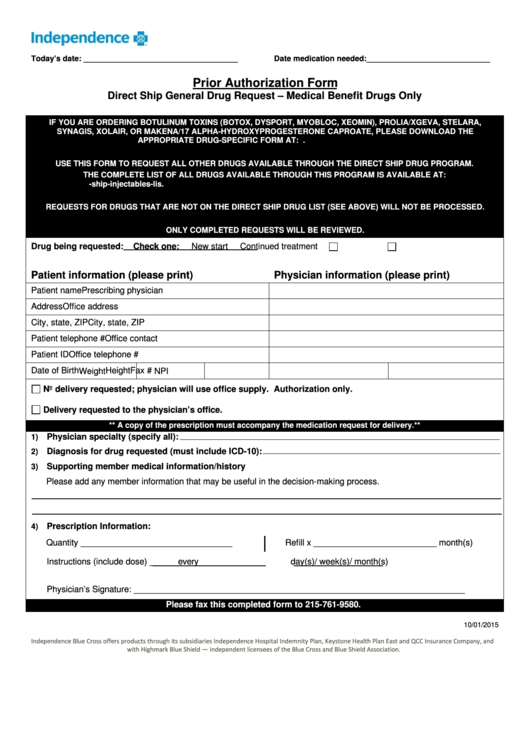
 Fillable Online Direct Ship Injectables Request Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Direct Ship Injectables Request Form Independence Blue Cross Fax Email Print Pdffiller
 New Anthem Blue Cross Blue Shield Prior Authorization Form For Radiology Models Form Ideas
New Anthem Blue Cross Blue Shield Prior Authorization Form For Radiology Models Form Ideas
 Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Https Ibx Com Pdfs Providers Pharmacy Information Prior Authorization Ibc Synvisc Pdf
 Fillable Online Prior Authorization Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Independence Blue Cross Fax Email Print Pdffiller
 Free 8 Prior Authorization Form Samples In Pdf Ms Word
Free 8 Prior Authorization Form Samples In Pdf Ms Word


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.