Kaiser Permanente offers private health insurance to residents of California Colorado Georgia Hawaii Oregon and Washington state as well as those living in Maryland Virginia Washington DC. Individual health plans are available through the Affordable Care Act ACA exchanges and outside the exchanges directly through insurance companies.
 Difference Between Individual Health Insurance Family Floater
Difference Between Individual Health Insurance Family Floater
Call our crisis response lines available to anyone in the US at 1-833-327-AETNA 1-833-327-2386 for.

Individual health insurance. You can also find additional insurance products to round out your coverage. Personal Health Insurance Plans. 7500 Security Boulevard Baltimore MD 21244.
Individual health insurance is coverage that you purchase on your own on an individual or family basis as opposed to obtaining through an employer or from a government-run program like Medicare Medicaid or CHIP. How Much Does an Individual Health Insurance Plan Cost. Were here to help make things less stressful for you.
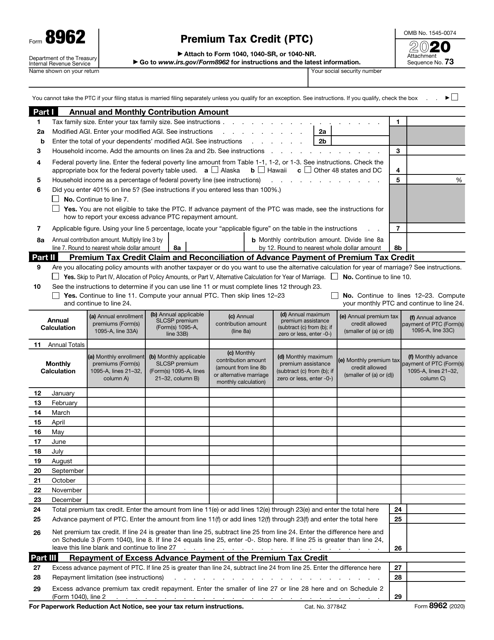
You may also qualify for a new higher premium tax credit and a cost-sharing reduction to help lower your health insurance premium and total out-of-pocket costs. Its network includes more than 23000 participating physicians. What is individual health insurance.
HealthMarkets offers a broad portfolio of health plans from recognized national and regional insurance companies. Individual and family plans Skip to. A federal government website managed and paid for by the US.
When retrieving a quote be sure to specify that youre. Updated on November 24 2020 In 2020 the average national cost for health insurance is 456 for an individual and 1152 for a family per month. How Much Does Individual Health Insurance Cost.
Plans for prior to age 65 or coverage to add on to other health insurance. Individual plans provide similar benefits as most employer plans. An individual health insurance plan only provides coverage for an individual whereas a family floater plan ensures coverage for the entire family in case of a medical emergency.
An individual health plan is one that is purchased with a single insured person in mind. On average the monthly health insurance premiums for individual plans is 440. However an individual plan costs more than a family health insurance floater plan which is why most individuals opt for family floaters.
If youre looking for individual or family health insurance prior to age 65 youll find UnitedHealthcare offers many choices to fit your needs. Group health insurance and health benefit plans are insured or administered by CHLIC Connecticut General Life Insurance Company. One of the biggest differences is that individual and family health insurance plans offered through the ACA receive subsidized premiums reducing the monthly cost of coverage.
Depending on your income you may pay even less for an individual health insurance plan than one through an employer. Typical health insurance plans for individuals include costs such as a monthly premium annual deductible copayments and coinsurance. Similar exemptions apply depending upon the policy which is bought.
This might be someone buying health insurance for themselves for their partner or. From platinum level metal plans to catastrophic only were ready to help you find a plan to fit your lifestyle. Centers for Medicare Medicaid Services.
Health Insurance Marketplace is a registered trademark of the Department of Health and Human Services. Family floaters also offer a higher sum. View individual and family plans near you.
During the 2021 Special Enrollment Period you can enroll in an individual and family health insurance plan without a qualifying event such as job loss or birth of a child. UnitedHealthCare has a large chosen supplier network of over 790000 participating doctors. Individual and family medical and dental insurance plans are insured by Cigna Health and Life Insurance Company CHLIC Cigna HealthCare of Arizona Inc Cigna HealthCare of Illinois Inc and Cigna HealthCare of North Carolina Inc.
Another difference is that you can only sign up for ACA health insurance during the open enrollment period usually late fall or due to a qualifying life event such as. The cost of your health insurance plan could be affected by age and tobacco use but you will not be declined for an individual health insurance plan due to pre-existing conditions. Plans for people before age 65 and coverage to add on to other health insurance.
However costs vary among the wide selection of health plans. You need to find affordable health insurance for yourself that fits your individual needs and budget.